Nursing Student - Blog Posts
Pulmonary Edema

Introduction
Pulmonary edema is a condition that results from the abnormal accumulation of fluid in the lungs, leading to impaired gas exchange and respiratory distress. This comprehensive discourse aims to provide an in-depth analysis of pulmonary edema, covering its pathophysiology, etiology, clinical manifestations, diagnostic modalities, treatment strategies, prevention strategies, and associated complications.
Pathophysiology of Pulmonary Edema

Pulmonary edema develops when there is an imbalance between the hydrostatic and oncotic pressures within the pulmonary vasculature. This imbalance leads to an increase in capillary permeability and the extravasation of fluid into the interstitial space and alveoli of the lungs. Several mechanisms contribute to this process, including increased capillary hydrostatic pressure due to heart failure, increased vascular permeability due to inflammation or injury, and decreased oncotic pressure due to hypoalbuminemia or capillary leak syndrome.
Etiology of Pulmonary Edema
The etiology of pulmonary edema can be categorized into cardiogenic and noncardiogenic causes. Cardiogenic pulmonary edema occurs secondary to heart failure or other cardiac conditions that result in elevated left atrial pressure and pulmonary venous congestion. Noncardiogenic pulmonary edema, on the other hand, is caused by factors unrelated to heart dysfunction, such as acute respiratory distress syndrome (ARDS), aspiration, sepsis, or neurogenic pulmonary edema.
Clinical Manifestations of Pulmonary Edema

The clinical presentation of pulmonary edema varies depending on the underlying cause and severity of the condition. Common symptoms include dyspnea, orthopnea, paroxysmal nocturnal dyspnea, cough, frothy sputum, cyanosis, and crackles on auscultation. Severe cases may progress to respiratory failure, hypoxemia, and hemodynamic instability.
Diagnostic Modalities for Pulmonary Edema

Diagnosing pulmonary edema requires a thorough clinical evaluation, including a detailed medical history, physical examination, and various diagnostic tests. Imaging studies such as chest X-ray, computed tomography (CT) scan, and lung ultrasound can provide valuable information about lung parenchymal changes and the presence of pulmonary congestion. Laboratory tests, including arterial blood gas analysis, brain natriuretic peptide levels, and electrolyte measurements, may also aid in the diagnosis and assessment of disease severity.
Treatment Strategies for Pulmonary Edema
The management of pulmonary edema involves addressing the underlying cause, relieving symptoms, and preventing complications. Initial treatment often includes supplemental oxygen therapy to improve oxygenation and reduce respiratory distress. Diuretics, such as furosemide or bumetanide, are commonly used to reduce fluid overload and alleviate pulmonary congestion. In cases of cardiogenic pulmonary edema, vasodilators, inotropes, or mechanical ventilation may be necessary to improve cardiac function and gas exchange.
Prevention Strategies for Pulmonary Edema
Preventing pulmonary edema requires a broad approach aimed at managing underlying risk factors and promoting healthy lifestyle habits. Patients with known cardiac conditions should adhere to prescribed medications, maintain a low-sodium diet, and monitor fluid intake to prevent fluid retention and exacerbation of heart failure. Individuals at risk of noncardiogenic pulmonary edema should avoid exposure to toxins, practice proper respiratory hygiene, and seek prompt medical attention for respiratory infections or injuries.
Complications of Pulmonary Edema

Untreated or inadequately managed pulmonary edema can lead to several complications, including acute respiratory distress syndrome (ARDS), cardiogenic shock, acute kidney injury, pulmonary hypertension, and death. Prompt recognition and intervention are essential to prevent progression to these life-threatening complications and improve patient outcomes.
Conclusion
Pulmonary edema is a complex and potentially life-threatening condition that requires prompt recognition, accurate diagnosis, and appropriate management. By understanding the underlying pathophysiology, etiology, clinical manifestations, diagnostic modalities, treatment strategies, prevention strategies, and associated complications of pulmonary edema, healthcare providers can optimize patient care and outcomes. Continued research efforts aimed at elucidating the mechanisms underlying pulmonary edema and identifying novel therapeutic targets are essential to further improve patient outcomes and reduce the global burden of this condition.
Embarking on your journey in the field of medicine is both exciting and challenging. As you navigate through your rigorous study period, it’s essential to seek guidance and assistance whenever needed to ensure your success.
At Expert Academic Assignment Help, we understand the demands of medical education and are here to support you every step of the way. Whether you require assistance with assignments, research papers, or exam preparation, our team of experts is dedicated to providing you with the help you need to excel in your studies.
Don’t hesitate to reach out to us for guidance, academic support, or any questions you may have. You can contact us via email at expertassignment46@gmail.com
6 Simple Steps To Score ‘A’ Grade On Your Research Paper

1. Building Your Thesis
Your thesis serves as the bedrock of your research paper, providing a central focus and guiding principle for your investigation. It’s imperative to construct your thesis around a clear and concise idea, premise, or claim that you intend to explore and defend throughout your paper. In the introduction, articulate precisely what your thesis aims to address, ensuring clarity and coherence from the start outlining the scope and significance of your thesis, you not only distinguish your paper from others but also establish a compelling rationale for your research. Moreover, show case to your readers the insights they stand to gain by engaging with your thesis, thereby enhancing the relevance and impact of your work.
2. Preparing an Outline

Crafting a comprehensive outline is an indispensable organizational tool in the research paper writing process. It functions as a strategic roadmap, enlightening the structure and content of your paper while facilitating coherence and logical progression. While there is no one-size-fits-all approach to outlining, it is essential to consider several key elements:
Content and Presentation Style: Determine the thematic framework and narrative structure for each section of your paper, ensuring alignment with your thesis.
Supporting Arguments and Evidence: Incorporate pertinent supporting arguments and empirical evidence to substantiate your thesis and bolster your overrating argument.
Cohesion and Conclusion: Ensure that your outline fosters cohesion by integrating disparate ideas and perspectives, culminating in a definitive conclusion that reinforces the significance of your research.
By vividly crafting an outline that contains these elements, you can streamline the writing process and maintain a cohesive and compelling narrative throughout your paper.
3. Conducting Research

Robust and thorough research is the cornerstone of a successful research paper, providing the empirical foundation and scholarly context necessary to substantiate your thesis. Begin by identifying a diverse array of potential sources that align with the theme focus and research objectives of your paper. With your outline serving as a strategic guide, embark on a systematic exploration of relevant literature, primary sources, and empirical data, prioritizing depth and breadth of coverage over superficiality. While evaluating sources, prioritize relevance and scholarly vigor over perfection, recognizing that the synthesis of diverse perspectives and methodologies can enrich your analysis and deepen the intellectual resonance of your paper.
4 . Writing Your Thesis

Armed with a comprehensive outline and an extensive body of research, it is time to translate your insights and arguments into a cognitive and compelling thesis. Drawing upon the scaffolding provided by your outline, into details craft each section of your paper, maintaining specificity to your thesis statement and overrated argument. Whether elucidating theoretical frameworks, analyzing empirical data, or synthesizing disparate perspectives, strive for consistency and coherence in your writing, ensuring that each subsection contributes meaningfully to the specific narrative of your paper. By adhering to the theme contours mentioned in your outline and showing the resilience of your thesis, you can construct a persuasive and intellectually rigorous argument that resonates with your readers.
5. Editing and Revision

The editing and revision process is an indispensable stage in refining the coherence, clarity, and scholarly rigor of your research paper. Upon completing the initial draft of your paper, undertake a comprehensive review and analysis, focusing on several key areas:
Structural Coherence: Evaluate the organizational coherence and logical progression of your paper, identifying opportunities to streamline transitions and enhance narrative flow.
Clarity and Precision: Scrutinize the clarity and precision of your prose, refining language and syntax to elucidate complex ideas and facilitate reader comprehension.
Scholarly Rigor: Verify the accuracy and integrity of your citations, ensuring adherence to established conventions of academic citation and attribution.
Grammar and Mechanics: Attend to grammatical errors, typographical inconsistencies, and syntactical ambiguities, rectifying any lapses in mechanics that deter from the scholarly integrity of your paper.
By subjecting your paper to rigorous scrutiny and revision, you can elevate the quality and scholarly resonance of your research, enhancing its capacity to engage and persuade your audience.
6. Creating a Checklist

As a culminating step, it is essential to create a comprehensive checklist to ensure that your research paper adheres to the highest standards of scholarly rigor and integrity. This checklist should encompass several key dimensions:
Content: Verify that your paper addresses all requisite components, including an introduction, literature review, methodology, findings, discussion, and conclusion.
Structure: Assess the structural coherence and narrative progression of your paper, ensuring that each section contributes meaningfully to the overarching argument.
Citation and Attribution: Confirm the accuracy and completeness of your citations, adhering to established conventions of academic citation and attribution.
Presentation: Review the formatting and presentation of your paper, attending to stylistic considerations such as font, spacing, and margins.
Proofreading: Conduct a final proofreading of your paper, scrutinizing for any lingering errors or oversights in grammar, syntax, or mechanics.
By rigorously adhering to this checklist, you can ensure that your research paper meets all necessary criteria for scholarly excellence and academic integrity, thereby maximizing its impact and credibility within the academic community.
By specifically following these six steps, you can consistently produce research papers of exceptional quality and academic rigor, irrespective of your current skill level or disciplinary background. Each step represents a critical juncture in the research paper writing process, providing a strategic framework for conceptualizing, organizing, and presenting your research in a compelling and intellectually rigorous manner. By embracing these principles and methodologies, you can elevate the caliber and excellent resonance of your research papers, thereby enhancing your academic proficiency and contributing meaningfully to the advancement of knowledge within your chosen field of study.
Crafting a top-notch research paper demands careful planning, thorough research, and diligent editing. Following the outlined steps can boost students’ writing skills and consistently lead to ‘A’ grades. Yet, academic writing complexities can overwhelm newcomers or those short on time.
Remember, seeking help isn’t weakness but a proactive strategy to ensure work quality. By utilizing available resources and seeking aid when necessary, students can ease academic writing stress and enrich their learning journey.
Therefore, I strongly encourage students to consider seeking assistance from Expert Academic Assignment Help by emailing expertassignment46@gmail.com With their expertise and support, students can receive tailored guidance, feedback, and assistance throughout the research paper writing process. By leveraging the expertise of academic professionals, students can overcome challenges, refine their writing skills, and achieve academic success more effectively.
What Is A Psychotic Disorders?

Introduction
Understanding psychotic disorders requires or encompassing various aspects such as types, symptoms, causes, diagnosis, treatment, prognosis, and preventive measures. Psychotic disorders constitute a diverse array of severe mental illnesses characterized by profound disturbances in cognition, emotion, communication, and behavior, significantly impairing individuals’ ability to function in daily life. Despite the gravity of these conditions, advancements in treatment modalities offer hope for recovery and effective management.
Types of Psychotic Disorders
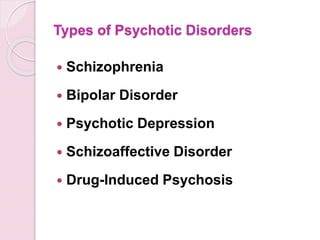
Schizophrenia
This debilitating disorder is characterized by profound alterations in behavior, delusions, and hallucinations persisting for at least six months. It exerts a profound impact on work, relationships, and overall functioning.
Schizoaffective Disorder
Combining features of schizophrenia with mood disorder symptoms like depression or bipolar disorder, schizoaffective disorder presents diagnostic and therapeutic challenges due to its complex symptomatology.
Schizophreniform Disorder
Resembling schizophrenia but with a shorter duration of symptoms (between one to six months), schizophreniform disorder provides insights into the acute phases of psychotic episodes.
Bipolar Psychotic Disorder
Individuals experience sudden, transient episodes of psychotic behavior, often precipitated by extreme stressors, with rapid recovery typically within a month.
Delusional Disorder
Centered around fixed false beliefs (delusions) concerning real-life situations, delusional disorder significantly influences perception and behavior, persisting for at least one month.
Shared Psychotic Disorder
Occurring when one individual’s delusion influences another within a close relationship, shared psychotic disorder elucidates the complexities of interpersonal dynamics in psychosis.
Substance-Induced Psychotic Disorder
Resulting from substance use or withdrawal, this condition underscores the intricate interplay between substance abuse and mental health.
Psychotic Disorder Due to Another Medical Condition
Hallucinations and delusions may arise secondary to underlying medical conditions affecting brain function, necessitating comprehensive evaluation and management.
Paraphrenia
Although not formally recognized in DSM-5, paraphrenia shares similarities with schizophrenia or delusional disorder and typically manifests in late adulthood, potentially associated with neurological factors.
Symptoms of Psychotic Disorders

Hallucinations
Involving perceptual experiences of stimuli that are not present in reality, hallucinations can manifest as auditory, visual, olfactory, gustatory, or tactile phenomena.
Delusions
These fixed, false beliefs persist despite evidence to the contrary, often revolving around themes of persecution, grandiosity, or paranoia.
Disorganized Thinking
Characterized by disjointed or incoherent thought processes, disorganized thinking manifests as impaired logical reasoning, tangential speech, or flight of ideas.
Bizarre Behavior
Individuals with psychotic disorders may exhibit unconventional or socially inappropriate behaviors, including agitation, catatonia, or unusual motor mannerisms.
Social Withdrawal
A hallmark feature of psychotic disorders is the withdrawal from social interactions and activities, often accompanied by a diminished interest in personal hygiene and self-care.
Mood Disturbances
Psychotic disorders may co-occur with mood symptoms such as depression or mania, further complicating the clinical presentation and treatment approach.
Causes of Psychotic Disorders

Genetic Predisposition
While genetic factors contribute to the risk of developing psychotic disorders, the inheritance pattern is complex, involving multiple genes and environmental interactions.
Environmental Factors
Stressful life events, trauma, childhood adversity, and substance abuse play significant roles in precipitating psychotic episodes and exacerbating symptoms.
Neurobiological Abnormalities
Dysregulation of neurotransmitters, particularly dopamine and glutamate, is implicated in the pathophysiology of psychotic disorders, affecting brain regions involved in cognition, perception, and emotion.
Diagnosis of Psychotic Disorders

A comprehensive diagnostic assessment involves obtaining a detailed medical and psychiatric history, conducting a thorough physical examination, performing laboratory tests to rule out medical conditions, and utilizing standardized psychiatric interviews and assessment tools.
Treatment of Psychotic Disorders

Medication
Antipsychotic medications are the cornerstone of pharmacological treatment, targeting symptoms such as delusions, hallucinations, and disorganized thinking. First-generation (typical) and second-generation (atypical) antipsychotics are prescribed based on efficacy and tolerability profiles, with newer agents offering improved side effect profiles and long-acting formulations enhancing treatment adherence.
Psychotherapy
Various forms of psychotherapy, including cognitive-behavioral therapy supportive therapy, and family therapy, complement pharmacotherapy by addressing psychosocial factors, enhancing coping skills, and improving functional outcomes.
Hospitalization
In severe cases or during acute psychotic episodes, hospitalization may be necessary to ensure safety, stabilize symptoms, and initiate intensive treatment interventions.
Prognosis and Recovery
The prognosis of psychotic disorders varies widely among individuals, influenced by factors such as early intervention, treatment adherence, social support, and the presence of comorbid conditions. While some individuals experience rapid symptom improvement and functional recovery, others may require long-term treatment and ongoing support to achieve stability and prevent relapse.
Prevention of Psychotic Disorders

Although prevention of psychotic disorders remains challenging, early intervention, identification of high-risk individuals, and mitigation of modifiable risk factors such as substance abuse and stress can reduce the incidence and severity of psychotic episodes. Public education, de stigmatization efforts, and access to mental health services promote awareness and facilitate timely intervention.
In conclusion, psychotic disorders represent complex and mental illnesses that profoundly impact individuals’ lives and necessitate comprehensive evaluation and treatment. By addressing the diverse array of symptoms, underlying neurobiological abnormalities, and psychosocial factors, clinicians can optimize treatment outcomes and support individuals in achieving improved quality of life and functioning. Through ongoing research, education, and advocacy, the understanding and management of psychotic disorders continue to evolve, offering hope for enhanced outcomes and reduced burden on affected individuals and society as a whole.
Students immersed in the fields of medical and psychology, seeking guidance from Expert Academic Assignment Help can be transformative. Whether it’s for assignments, studies, or navigating the challenges of medical School, expert assistance can provide clarity, direction, and invaluable insights. By reaching out to expertassignment46@gmail.com students can access personalized support, comprehensive resources, and expert advice to excel in their academic pursuits and lay a solid foundation for their future careers. Don’t hesitate to seek guidance — your academic success and professional growth are worth investing in.
Cirrhosis Of The Liver

Introduction
Cirrhosis stands as a challenge in the narrative of liver disease, marking the culmination of a complex interplay of factors that converge to undermine the organ’s structural integrity and functional capacity. This condition, characterized by the progressive accumulation of scar tissue within the liver parenchyma, holds a cascade of physiological network that reverberate throughout the body, manifesting in a spectrum of symptoms and complications. From its inner onset to its profound implications for morbidity and mortality, cirrhosis generate the intricate interplay between genetic predisposition, environmental influences, and individual behaviors.
In this comprehensive discussion, we embark on an exploration of the multifaceted dimensions of cirrhosis, traversing its etiological underpinnings, clinical manifestations, diagnostic modalities, therapeutic strategies, and avenues for prevention and self-care. By delving into the intricacies of cirrhosis, we endeavor to elucidate the imperative of early recognition, proactive intervention, and holistic management in ameliorating its adverse sequelae and fostering optimal outcomes for affected individuals
Pathophysiology of Cirrhosis

Central to the pathogenesis of cirrhosis lies a complex interplay of molecular and cellular events that precipitate the gradual transformation of healthy hepatic tissue into fibrotic scar tissue. At the heart of this process lies fibrogenesis, wherein a multitude of cellular players, including hepatic stellate cells, inflammatory mediators, and extracellular matrix proteins, triggers a profibrotic milieu in response to persistent liver injury and inflammation. The ensuing deposition of collagen-rich scar tissue disrupts the structure of the liver lobules, impeding normal hepatocellular function and vascular dynamics.
Symptoms and Clinical Manifestations

The clinical presentation of cirrhosis spans a broad spectrum, reflecting the diverse array of physiological derangements engendered by advanced liver disease. Early-stage cirrhosis may manifest subtly, with nonspecific symptoms such as fatigue, malaise, and vague abdominal discomfort, often eluding timely diagnosis. However, as the disease progresses, overt signs of hepatic decompensation emerge, including jaundice, ascites, hepatic encephalopathy, and gastrointestinal bleeding, heralding the onset of life-threatening complications. Moreover, cirrhosis exerts systemic effects beyond the confines of the liver, precipitating coagulopathy, renal dysfunction, and metabolic disturbances.
Etiology and Risk Factors
Cirrhosis arises from an influence of etiological insults, encompassing a diverse spectrum of predisposing factors that contribute to hepatocellular injury and fibrogenesis. Foremost among these is chronic alcohol abuse, which inflicts direct hepatotoxic effects and potentiates oxidative stress and inflammatory cascades within the liver microenvironment. Additionally, viral hepatitis infections, particularly hepatitis B and C, constitute major drivers of cirrhosis worldwide, underscoring the imperative of vaccination and antiviral therapy in disease prevention and management. Other contributing factors include nonalcoholic fatty liver disease, autoimmune disorders, hereditary hemochromatosis, and biliary tract diseases, each exerting a unique influence on cirrhosis pathogenesis.
Diagnostic Modalities

Accurate diagnosis forms the linchpin of effective cirrhosis management, necessitating a judicious amalgamation of clinical symptoms, laboratory investigations, imaging modalities, and histopathological evaluation. Liver function tests serve as indispensable tools for gauging the synthetic and metabolic capacity of the liver, while imaging studies such as ultrasound, computed tomography (CT), and magnetic resonance imaging (MRI) afford insights into hepatic morphology, vascular dynamics, and the presence of focal lesions. Despite their utility, these modalities may be supplemented by liver biopsy, which remains the gold standard for assessing the degree of fibrosis and guiding therapeutic decisions, albeit fraught with procedural risks and sampling variability.
Treatment Strategies

While cirrhosis represents a chronic and irreversible condition, therapeutic interventions are geared toward monitoring disease progression, alleviating symptoms, and forestalling the onset of complications. Pharmacological therapies, including hepatoprotective agents, antifibrotic agents, and symptom-based medications, aim to attenuate hepatic inflammation, inhibit fibrogenesis, and ameliorate symptom burden in cirrhotic patients. Furthermore, endoscopic interventions such as variceal band ligation and trans jugular intrahepatic portosystemic shunting play a major role in the management of portal hypertension and its sequelae, including variceal bleeding and refractory ascites. For select individuals with end-stage liver disease, liver transplantation offers a definitive therapeutic option, affording a second lease on life and circumventing the inexorable progression of cirrhosis-related complications.
Self-Care and Lifestyle

Empowering individuals with cirrhosis to adopt proactive self-care measures constitutes a cornerstone of comprehensive disease management, emphasizing the role of lifestyle modifications, dietary interventions, and preventive strategies in optimizing health outcomes. Lifestyle modifications, including abstinence from alcohol, adherence to a liver-friendly diet, regular exercise, and smoking cessation, are paramount in attenuating hepatic inflammation, promoting metabolic homeostasis, and mitigating cardiovascular risk factors in cirrhotic patients. Additionally, vaccination against hepatitis viruses, avoidance of hepatotoxic medications, and judicious monitoring of comorbid conditions serve as essential pillars of preventive care, safeguarding against disease exacerbations and fostering long-term wellness in individuals with cirrhosis.
Conclusion
Cirrhosis emerges as a complex and a dangerous disease, syndrome characterized by progressive hepatic fibrosis, compromised organ function, and a plethora of systemic manifestations. The etiological heterogeneity of cirrhosis underscores the need for a personalized and multidisciplinary approach to disease management, Focusing to the unique pathophysiological mechanisms and clinical manifestations inherent to each individual. Through timely diagnosis, targeted interventions, and collaborative care, healthcare providers can mitigate the burden of cirrhosis, optimize patient quality of life, and prolong survival in affected individuals. As we navigate complexities of cirrhosis, a concerted emphasis on preventive measures, patient education, and therapeutic innovations holds the key to unlocking a brighter prognosis for those afflicted by this formidable liver disease.
Medical students encounter significant academic challenges during their studies, balancing coursework, clinical rotations, research, and personal commitments. Expert Academic Assignment Help offers tailored assistance to meet their needs, providing study materials, tutoring, assignment help, and exam preparation. Beyond academics, it fosters a supportive environment for mentorship and guidance. In essence, Expert Academic Assignment Help is a valuable resource for medical students, empowering them to excel academically and develop into competent healthcare professionals. Contact at expertassignment46@gmail.com for assistance guidance.
Diabetes

Introduction to Diabetes
Diabetes, a metabolic disorder characterized by chronic hyperglycemia, arises from abnormalities in insulin secretion, insulin action, or both. The condition’s prevalence has reached epidemic proportions globally, with significant health, economic, and social implications.
Types of Diabetes

Type 1 Diabetes: This autoimmune disease results from the destruction of pancreatic beta cells, leading to absolute insulin deficiency. Genetics and environmental triggers play pivotal roles in its pathogenesis. Despite being less common than Type 2 diabetes, its onset during childhood or adolescence significantly impacts individuals’ lives.
Type 2 Diabetes: Predominantly a disorder of insulin resistance, Type 2 diabetes accounts for the majority of diabetes cases worldwide. Lifestyle factors, genetic predisposition, and obesity contribute to its development. Its insidious onset often leads to delayed diagnosis and increased risk of complications.
Gestational Diabetes: Occurring during pregnancy, gestational diabetes poses risks to both maternal and fetal health. Hormonal changes and insulin resistance characterize its pathophysiology. Effective screening and management are crucial to prevent adverse outcomes.
Other Types of Diabetes: Variants like MODY, LADA, and secondary diabetes present unique challenges in diagnosis and management, requiring tailored approaches to care.
Epidemiology and Prevalence
Diabetes prevalence varies across demographics, with disparities observed in age, gender, ethnicity, and socioeconomic status. The escalating burden of diabetes underscores the urgent need for targeted prevention and management strategies.
Symptoms and Causes

Hyperglycemia-induced symptoms like polyuria, polydipsia, and unexplained weight loss serve as clinical indicators for diabetes diagnosis. Understanding the complex interplay of genetic, environmental, and lifestyle factors elucidates the condition’s etiology.
Complications
Diabetes complications encompass a spectrum of microvascular and macrovascular disorders, significantly impacting quality of life and life expectancy. From diabetic retinopathy to cardiovascular disease, nephropathy, neuropathy, and diabetic foot complications, the ripple effects of uncontrolled diabetes are profound.
Diagnosis and Tests

Accurate diagnosis relies on comprehensive evaluation, including fasting glucose, oral glucose tolerance tests, and hemoglobin A1c measurements. Screening recommendations aim to identify at-risk individuals early, facilitating timely intervention and risk reduction.
Management and Treatment
Diabetes management strategies encompass pharmacotherapy, lifestyle modifications, patient education, and multidisciplinary care. Individualized treatment plans address glycemic control, blood pressure management, lipid optimization, and prevention of complications.
Prevention
Prevention initiatives target modifiable risk factors through health promotion, public health interventions, and community engagement. Emphasizing the role of nutrition, physical activity, and behavioral changes empowers individuals to mitigate their diabetes risk.
Outlook and Prognosis
Prognostic factors such as glycemic control, adherence to therapy, comorbidity burden, and psychosocial support influence long-term outcomes. Enhanced collaboration among healthcare providers, policymakers, and stakeholders is essential to improve diabetes prognosis globally.
Living With Diabetes

Coping with diabetes requires resilience, self-management skills, and social support networks. Empowering individuals through education, self-monitoring tools, and peer support enhances their capacity to navigate the challenges of daily diabetes management.
Impact on Individuals and Society
Diabetes exerts a profound socioeconomic burden, encompassing healthcare costs, productivity losses, and reduced quality of life. Addressing the psychosocial dimensions of diabetes care is integral to fostering holistic well-being and societal resilience.
Future Directions and Research

Advancements in diabetes research, including precision medicine, digital health technologies, and novel therapeutics, offer promising avenues for disease management and prevention. Collaborative research endeavors aim to translate scientific discoveries into tangible clinical benefits.
Conclusion
In conclusion, diabetes represents public health challenge necessitating a comprehensive, patient-centered approach. By fostering awareness, promoting early detection, and advancing evidence-based interventions, we can mitigate the impact of diabetes on individuals, families, and communities worldwide.
Medical students encounter significant academic challenges during their studies, balancing coursework, clinical rotations, research, and personal commitments. Expert Academic Assignment Help offers tailored assistance to meet their needs, providing study materials, tutoring, assignment help, and exam preparation. Beyond academics, it fosters a supportive environment for mentorship and guidance. In essence, Expert Academic Assignment Help is a valuable resource for medical students, empowering them to excel academically and develop into competent healthcare professionals. Contact at expertassignment46@gmail.com for assistance.
How to Write a Case Study

Introduction
The case study indulges into the ideal process of rehabilitating a semi-professional cyclist who underwent a traumatic transfemoral amputation due to a road traffic accident. This comprehensive analysis aims to shed light on the complexities of limb loss rehabilitation, emphasizing the importance of tailored interventions and evidence-based practice in optimizing outcomes for individuals facing similar challenges.
Client Characteristics
In this section, a detailed exploration of the patient’s background, lifestyle, and medical history provides crucial insights into his unique rehabilitation needs. Emphasis is placed on the impact of the accident on the patient’s physical and psychological well-being, as well as his aspirations for returning to an active lifestyle post-amputation.
The patient, a previously healthy 24-year-old male, was actively engaged in semi-professional cycling and held a physically demanding job at a bicycle shop. The road traffic accident resulted in a traumatic transfemoral amputation, significantly altering his physical capabilities and emotional state. His aspirations to return to his previous level of physical activity underscore the importance of addressing both the physical and psychological aspects of his rehabilitation journey.
Examination Findings
A thorough examination is conducted to assess the patient’s physical condition and identify areas of impairment resulting from the amputation. Objective measurements, including strength assessments and gait analysis, complement subjective reports of phantom limb pain and functional limitations, forming the basis for the subsequent formulation of a clinical hypothesis.
The examination reveals significant impairments in strength and mobility, as well as the presence of phantom limb pain, which negatively impacts the patient’s daily life and rehabilitation progress. These findings highlight the need for a comprehensive treatment approach that addresses both the physical and psychological aspects of the patient’s condition.
Clinical Hypothesis/Impression
Drawing on current research and clinical expertise, the clinical hypothesis focuses on addressing the patient’s complex pain experience and psychological distress following the amputation. The identification of neuropathic pain mechanisms and the potential efficacy of interventions such as mirror therapy and mental imagery inform the development of a tailored treatment plan aimed at promoting pain relief and enhancing functional recovery.
The clinical hypothesis highlights the importance of addressing the underlying causes of the patient’s pain and implementing evidence-based interventions to optimize his rehabilitation outcomes. By targeting both the physical and psychological aspects of his condition, the treatment plan aims to improve the patient’s overall quality of life and facilitate his successful return to daily activities.
Intervention
The intervention plan is majorly crafted to address the patient’s unique rehabilitation goals and challenges. A multi-disciplinary approach, incorporating pharmacological interventions, prosthetic care, and psychological support, is implemented to optimize outcomes and empower the patient in his journey towards recovery. Detailed descriptions of specific treatment modalities and their rationale are provided, highlighting the importance of individualized care and ongoing monitoring throughout the rehabilitation process.
The intervention plan includes a combination of pharmacological management, prosthetic fitting and training, and psychological support to address the patient’s physical and psychological needs. Each component of the plan is tailored to the patient’s specific goals and challenges, with regular monitoring and adjustments made to ensure optimal outcomes.
Outcome
Objective measures are used to track the patient’s progress and evaluate the effectiveness of the intervention plan. Significant improvements in pain management, functional mobility, and quality of life are observed over the course of treatment, with particular emphasis on the transformative impact of mirror therapy on the patient’s pain experience and overall well-being. The importance of ongoing follow-up and support is emphasized as integral to maintaining long-term gains and facilitating the patient’s successful reintegration into daily activities.
The patient demonstrates significant improvements in pain management, functional mobility, and overall quality of life following the implementation of the intervention plan. Objective measures, including pain intensity ratings and functional assessments, demonstrate tangible improvements in the patient’s physical and psychological well-being, highlighting the effectiveness of the multi-disciplinary approach employed in his rehabilitation.
Discussion
A comprehensive discussion examines the broader implications of the case study for physiotherapy practice, highlighting the importance of holistic rehabilitation approaches that address the complex interplay of physical, psychological, and social factors in individuals with limb loss. Key lessons learned from the case study, including the value of evidence-based practice and the need for ongoing collaboration between healthcare professionals, are discussed in relation to optimizing outcomes and promoting patient-centered care.
The discussion explores the broader implications of the case study for physiotherapy practice, emphasizing the importance of adopting a holistic approach to rehabilitation that addresses the complex needs of individuals with limb loss. By integrating evidence-based interventions and fostering interdisciplinary collaboration, healthcare professionals can enhance the effectiveness of rehabilitation interventions and improve outcomes for patients with limb loss.
Conclusion
In conclusion, the extended case study provides a detailed exploration of the rehabilitation journey of a semi-professional cyclist following a traumatic limb amputation. Through a comprehensive analysis of client characteristics, examination findings, intervention strategies, and outcomes, valuable insights are gained into the complexities of limb loss rehabilitation and the importance of personalized, evidence-based care in achieving optimal outcomes for individuals facing similar challenges.
The case study underscores the importance of adopting a holistic approach to rehabilitation that addresses the physical, psychological, and social aspects of limb loss by focusing on interventions to the unique needs of each patient and fostering interdisciplinary collaboration, healthcare professionals can optimize outcomes and improve the quality of life for individuals with limb loss.
As academic students and researchers navigate the challenges of their assignments and research endeavors, Expert Academic Assignment Help stands ready to provide professional guidance and assistance. Whether you require support with assignment writing, research paper assistance, or essay help, our team of experts is dedicated to helping you achieve academic excellence. Reach out to us today at expertassignment46@gmail.com and let us support you on your academic journey. We wish you success and professional excellence.
H. pylori Infection

Introduction
Helicobacter pylori (H. pylori) infection is a significant global health concern, affecting a substantial portion of the world’s population. The discussion aims to provide an in-depth exploration of various aspects of H. pylori infection, including its prevalence, transmission, symptoms, diagnosis, treatment, complications, prevention strategies, and future research directions.
Prevalence and Transmission

H. pylori infection is widespread, with approximately two-thirds of the world’s population harboring the bacterium in their gastrointestinal tract. Various factors contribute to its prevalence, including socioeconomic status, living conditions, hygiene practices, and geographic location. The discussion indulges into the epidemiological trends of H. pylori infection across different populations and regions, highlighting disparities in prevalence rates and associated risk factors.
Transmission of H. pylori occurs primarily through interpersonal contact and ingestion of contaminated food or water. Saliva, fecal-oral transmission, and oral-oral transmission, including through kissing, are significant modes of spread. Poor sanitation and overcrowded living conditions facilitate the transmission of the bacterium, particularly in resource-limited settings. The discussion explores the mechanisms of H. pylori transmission and the implications for public health interventions aimed at reducing its spread.
Symptoms and Diagnosis

While many individuals with H. pylori infection remain asymptomatic, others experience a range of gastrointestinal symptoms, including stomach pain, bloating, nausea, and weight loss. The discussion elucidates the spectrum of clinical manifestations associated with H. pylori infection, emphasizing the importance of recognizing atypical presentations and considering differential diagnoses.
Diagnosing H. pylori infection presents several challenges due to the variability of symptoms and the limitations of available diagnostic tests. We critically evaluates the utility of different diagnostic modalities, including stool antigen tests, urea breath tests, and upper gastrointestinal endoscopy, in detecting H. pylori infection. It also examines the role of serological tests and molecular techniques in enhancing diagnostic accuracy and guiding clinical management decisions.
Treatment Options

The standard treatment regimens for H. pylori infection typically involve a combination of antibiotics and proton pump inhibitors (PPIs). However, rising rates of antibiotic resistance pose significant challenges to effective eradication therapy. It explores the mechanisms of antibiotic resistance in H. pylori and the implications for treatment outcomes.
Alternative treatment approaches, such as sequential therapy, concomitant therapy, and bismuth-based quadruple therapy, are also examined in the context of their efficacy and tolerability. Highlighting the importance of individualizing treatment regimens based on antibiotic susceptibility testing and patient-specific factors to optimize therapeutic outcomes.
Complications

Peptic ulcers are a common complication of H. pylori infection, resulting from the bacterium’s ability to disrupt the gastric mucosal barrier and induce inflammation. The discussion elucidates the pathophysiology of peptic ulcer formation and the factors contributing to ulcer recurrence and complications.
In addition to peptic ulcers, H. pylori infection is associated with an increased risk of more serious complications, such as gastric cancer and mucosa-associated lymphoid tissue (MALT) lymphoma. The discussion explores the molecular mechanisms underlying H. pylori-induced carcinogenesis and the strategies for early detection and management of gastric neoplasms.
Prevention

Preventive measures play a crucial role in reducing the burden of H. pylori infection and its associated complications. The discussion emphasizes the importance of promoting good hygiene practices, including handwashing and sanitation, to minimize the risk of transmission.
Furthermore, dietary factors may influence the risk of H. pylori infection and its clinical outcomes. The discussion evaluates the evidence regarding the impact of dietary habits, such as consumption of fruits, vegetables, and probiotics, on H. pylori colonization and disease progression. It also addresses the potential role of vaccination in preventing H. pylori infection and its complications, highlighting ongoing research efforts in vaccine development.
Research and Future Directions
Ongoing research efforts are focused on advancing our understanding of H. pylori pathogenesis, identifying novel therapeutic targets, and developing effective preventive strategies. The discussion highlights recent advancements in H. pylori research, including insights into bacterial virulence factors, host immune responses, and microbial interactions within the gastric microbiota.
Future directions in H. pylori research encompass a multidisciplinary approach, integrating molecular biology, epidemiology, immunology, and clinical medicine. The discussion outlines key areas for future investigation, such as the development of targeted antimicrobial agents, the role of host genetics in H. pylori susceptibility, and the impact of microbial dysbiosis on disease outcomes.
Conclusion
In conclusion, H. pylori infection remains a significant public health challenge, with implications for gastrointestinal health and disease worldwide. A comprehensive understanding of the epidemiology, pathogenesis, diagnosis, treatment, and prevention of H. pylori infection is essential for guiding clinical practice and informing public health policies. By addressing the complexities of H. pylori infection through interdisciplinary research and collaborative efforts, we can strive towards reducing its global burden and improving patient outcomes.
In managing H. pylori infection, compassion, empathy, and a holistic approach are crucial alongside clinical expertise. Striving for excellence in knowledge and practice enables us to advance gastroenterology and improve patient outcomes.
As we address H. pylori infection and its broader implications on gastrointestinal health, let’s remain dedicated to providing optimal patient care. By working collaboratively and embracing interdisciplinary approaches, we can positively impact lives and contribute to a healthier future.
Email expertassignment46@gmail.com to explore how we can assist you in achieving your academic and professional aspirations. Wishing you continued success in your medical journey.
Pneumonia In Children And Adults

Introduction
Pneumonia stands as a prevalent respiratory infection, exerting a significant burden on global public health. Its impact extends beyond mere morbidity, contributing to substantial healthcare costs and socioeconomic consequences. This discussion aims to elucidate the general nature of pneumonia, encompassing its pathophysiology, clinical presentation, diagnostic modalities, treatment strategies, complications, and preventive measures. By indulging into these factors, we aim to provide a better understanding of pneumonia’s complexity and underscore the importance of timely recognition and management.
Pathophysiology

Pneumonia ensues from the infiltration of infectious agents, including bacteria, viruses, fungi, and less commonly, parasites, into the lower respiratory tract. Upon inhalation or aspiration of these pathogens, they gain access to the alveoli, where they incite an inflammatory response. This inflammatory cascade triggers the release of pro-inflammatory cytokines and chemokines, recruiting immune cells to the site of infection. Neutrophils, macrophages, and lymphocytes converge to eradicate the invading pathogens, leading to the characteristic consolidation and exudate formation within the affected lung tissue. As the infection progresses, alveolar edema, impaired gas exchange, and parenchymal damage ensue, culminating in the clinical manifestations of pneumonia.
Clinical Presentation

The clinical presentation of pneumonia encompasses a spectrum of symptoms, ranging from mild respiratory complaints to life-threatening respiratory failure. Common symptoms include cough, productive sputum production, fever, chills, pleuritic chest pain, dyspnea, tachypnea, and systemic manifestations such as malaise and fatigue. The severity of symptoms varies depending on factors such as the underlying pathogen, the extent of lung involvement, the host’s immune status, and comorbidities. In pediatric populations, pneumonia may present with nonspecific symptoms such as feeding difficulties, lethargy, and irritability, posing diagnostic challenges. Conversely, elderly individuals may exhibit atypical presentations characterized by confusion, hypothermia, and exacerbations of underlying chronic conditions.
Diagnostic Modalities

The diagnosis of pneumonia hinges on a comprehensive clinical assessment, augmented by various diagnostic modalities to confirm the presence of pulmonary infection and reveal its etiology. A thorough history and physical examination provide invaluable insights into the patient’s symptomatology, risk factors, and clinical trajectory. Symptomatic findings such as crackles, wheezes, and diminished breath sounds may aid in localizing the site of infection and assessing disease severity. Radiographic imaging, notably chest X-rays and computed tomography (CT) scans, serves as the cornerstone of pneumonia diagnosis, revealing characteristic radiographic findings such as airspace opacities, lobar consolidation, and interstitial infiltrates. Laboratory investigations, including complete blood count (CBC), C-reactive protein (CRP), and procalcitonin levels, may corroborate the clinical suspicion of pneumonia and guide therapeutic decisions. Additionally, microbiological testing of respiratory specimens through techniques such as sputum culture, blood cultures, and polymerase chain reaction (PCR) assays facilitates pathogen identification and antimicrobial susceptibility testing, thereby informing targeted therapy.
Treatment Strategies

The management of pneumonia hinges on prompt initiation of empiric antimicrobial therapy tailored to the likely causative pathogen(s) and disease severity. Antibiotics represent the mainstay of treatment for bacterial pneumonia, with the choice of agent dictated by factors such as local antimicrobial resistance patterns, patient age, comorbidities, and recent antibiotic exposure. Commonly prescribed antibiotics include beta-lactam agents (e.g., penicillins, cephalosporins), macrolides, fluoroquinolones, and combination regimens for severe or healthcare-associated infections. Conversely, viral pneumonia necessitates supportive care measures, given the limited efficacy of antiviral agents in most cases. Influenza-associated pneumonia may benefit from neuraminidase inhibitors such as oseltamivir, while respiratory syncytial virus (RSV) pneumonia may warrant ribavirin therapy in select cases. Adjunctive therapies such as oxygen supplementation, bronchodilators, and corticosteroids may mitigate respiratory distress and improve clinical outcomes, particularly in severe or hypoxemic patients. The duration of antimicrobial therapy varies depending on factors such as the causative pathogen, clinical response, radiographic resolution, and the presence of complications. Close monitoring of clinical parameters and serial imaging studies guide the decision-making process, enabling clinicians to tailor therapy to individual patient needs.
Complications

Pneumonia harbors the potential for various complications, ranging from mild to life-threatening sequelae, necessitating vigilant monitoring and timely intervention. Common complications include pleural effusion, empyema, lung abscess, respiratory failure, septic shock, and acute respiratory distress syndrome (ARDS). Pleural effusion denotes the accumulation of fluid within the pleural space, secondary to inflammation or impaired lymphatic drainage, manifesting as dyspnea, pleuritic chest pain, and dullness to percussion on physical examination. Empyema represents a purulent collection within the pleural cavity, often complicating bacterial pneumonia and necessitating drainage via thoracentesis or chest tube placement. Lung abscesses manifest as circumscribed cavities containing necrotic debris and pus within the lung parenchyma, triggered by persistent fever, productive cough, and hemoptysis. Respiratory failure ensues from impaired gas exchange and alveolar hypoventilation, caused by worsening hypoxemia, hypercapnia, and respiratory acidosis, necessitating mechanical ventilation and intensive care support. Septic shock represents a life-threatening complication of severe pneumonia, characterized by systemic inflammatory response syndrome (SIRS) and end-organ dysfunction, requiring aggressive fluid resuscitation, vasopressor therapy, and broad-spectrum antibiotics. ARDS denotes a severe form of acute lung injury, characterized by diffuse alveolar damage, refractory hypoxemia, and bilateral infiltrates on chest imaging, necessitating lung-protective ventilation and supportive care in the intensive care unit (ICU). The occurrence of complications portends a poor prognosis and underscores the need for early recognition and intervention to mitigate adverse outcomes.
Preventive Measures

Preventing pneumonia entails a broad approach encompassing vaccination, infection control measures, and health promotion strategies aimed at reducing the risk of respiratory infections and their sequelae. Vaccination stands as a cornerstone of pneumonia prevention, targeting common bacterial and viral pathogens implicated in pneumonia pathogenesis. Vaccines such as the pneumococcal conjugate vaccine (PCV13) and pneumococcal polysaccharide vaccine (PPSV23) confer protection against Streptococcus pneumoniae, the leading bacterial cause of pneumonia, particularly in high-risk populations such as young children, older adults, and immunocompromised individuals. Influenza vaccination remains paramount in mitigating influenza-associated pneumonia and reducing disease transmission, underscoring the importance of annual vaccination campaigns targeting vulnerable populations. Additionally, adherence to infection control measures, including hand hygiene, respiratory etiquette, and environmental sanitation, plays a pivotal role in reducing the spread of respiratory pathogens in healthcare settings and the community at large. Health promotion efforts aimed at smoking cessation, optimizing nutrition, and addressing underlying comorbidities such as chronic obstructive pulmonary disease (COPD), asthma, and immunodeficiency bolster immune resilience and mitigate pneumonia risk. Furthermore, early identification and management of predisposing factors such as malnutrition, homelessness, and overcrowded living conditions attenuate pneumonia susceptibility and enhance overall health outcomes.
Conclusion
In conclusion, pneumonia emerges as a formidable respiratory infection, posing significant challenges to global public health. Its diverse etiology, clinical manifestations, diagnostic modalities, treatment modalities, complications, and preventive measures underscore the nature of pneumonia management. Timely recognition and intervention are imperative in mitigating the morbidity and mortality associated with pneumonia, necessitating a collaborative approach among healthcare providers, public health authorities, and policymakers. By fostering a comprehensive understanding of pneumonia’s manifest and implementing evidence-based strategies, we can strive towards reducing its burden and improving patient outcomes. Through ongoing research, education, and advocacy efforts, we can envision a future where pneumonia-related morbidity and mortality are substantially diminished, paving the way for enhanced respiratory health and well-being worldwide.
In managing pneumonia, compassion, empathy, and a holistic approach are essential alongside clinical expertise. Striving for excellence in knowledge and practice allows us to enhance respiratory medicine and patient outcomes.
As we address pneumonia and broader cardiovascular health complexities, let’s remain committed to optimal patient care. Together, we can impact lives positively and foster a healthier future.
Email expertassignment46@gmail.com to discover how we can support your academic and professional goals. Wishing you ongoing success in your medical journey.
Atherosclerosis

Introduction
Atherosclerosis is a chronic and progressive condition characterized by the accumulation of plaque within the walls of arteries, leading to their hardening and narrowing. Despite being often asymptomatic in its early stages, atherosclerosis poses significant risks to cardiovascular health and can result in severe complications such as heart attacks, strokes, and peripheral artery disease (PAD). Therefore, comprehensive knowledge of its symptoms, causes, prevention strategies, diagnosis methods, and treatment options is imperative for effectively managing its impact on individuals’ well-being.
Symptoms of Atherosclerosis

Atherosclerosis typically advances silently, with symptoms only becoming apparent as arteries become significantly obstructed or when a cardiovascular event occurs. The manifestation of symptoms varies depending on the affected arteries, each presenting distinct clinical presentations:
Coronary Arteries: The narrowing of coronary arteries due to atherosclerosis can lead to symptoms such as arrhythmia (irregular heartbeat), angina (chest pain or pressure), and shortness of breath, especially during physical exertion.
Cerebral Arteries: Atherosclerosis affecting cerebral arteries may manifest as numbness or weakness in the limbs, difficulty speaking or understanding speech, drooping facial muscles, paralysis, severe headache, or vision problems, indicating a heightened risk of stroke.
3. Peripheral Arteries: Individuals with atherosclerosis in peripheral arteries may experience symptoms such as leg pain when walking (intermittent claudication), numbness, cold extremities, aching or burning sensations in the feet, and slow-healing wounds or infections, reflecting compromised blood flow to the extremities
4. Renal Arteries: Atherosclerosis affecting renal arteries can result in elevated blood pressure (hypertension) and eventual kidney failure, highlighting the systemic impact of arterial narrowing on vital organ function.
Causes and Stages of Atherosclerosis

The development and progression of atherosclerosis involve a series of intricate biological processes initiated by damage to the endothelium, the delicate inner lining of arteries. As plaque composed of cholesterol, fat, calcium, and inflammatory substances accumulates within arterial walls, the disease progresses through distinct stages:
Damage to the Endothelium: The initial stage of atherosclerosis is characterized by injury to the endothelial cells lining the arteries, often attributed to risk factors such as high cholesterol, hypertension, inflammation, obesity, diabetes, and smoking.
2. Formation of Fatty Streaks: Following endothelial damage, the infiltration of low-density lipoprotein (LDL) cholesterol into the arterial wall triggers an inflammatory response, leading to the formation of fatty streaks — the earliest visible signs of atherosclerosis.
3 . Development of Fibrous Plaques: Over time, the accumulation of cholesterol-laden foam cells and the proliferation of smooth muscle cells contribute to the formation of fibrous plaques, which protrude into the arterial lumen and impede blood flow.
4 . Formation of Complicated Lesions: Advanced atherosclerosis is characterized by the formation of complicated lesions, where unstable plaques prone to rupture expose thrombogenic components, leading to the formation of blood clots and subsequent cardiovascular events such as myocardial infarction or ischemic stroke.
Risk Factors for Atherosclerosis
Numerous modifiable and non-modifiable risk factors influence the development and progression of atherosclerosis, underscoring the multifactorial nature of the disease. These risk factors include:
High Cholesterol: Elevated levels of LDL cholesterol, commonly referred to as “bad” cholesterol, promote the deposition of cholesterol within arterial walls, contributing to plaque formation and atherosclerosis progression.
2. High Blood Pressure: Hypertension exerts mechanical stress on arterial walls, accelerating endothelial damage and promoting atherosclerosis development
3. Inflammation: Chronic inflammatory conditions, such as rheumatoid arthritis or systemic lupus erythematosus, exacerbate endothelial dysfunction and foster plaque formation within arteries.
4. Obesity: Excess adiposity predisposes individuals to metabolic abnormalities, including dyslipidemia and insulin resistance, which fuel atherosclerosis progression.
5. Diabetes: Both type 1 and type 2 diabetes mellitus increase the risk of atherosclerosis by inducing endothelial dysfunction, promoting inflammation, and accelerating the formation of advanced glycation end-products (AGEs) implicated in vascular
6. Smoking: Tobacco smoke contains toxic compounds that promote endothelial injury, oxidative stress, and inflammation, exacerbating the progression of atherosclerosis and increasing the risk of cardiovascular events.
7.Sedentary Lifestyle: Physical inactivity contributes to metabolic derangements, including obesity, dyslipidemia, and insulin resistance, fostering atherosclerosis development and cardiovascular risk.
8. Family History of Heart Disease: Genetic predisposition plays a significant role in atherosclerosis susceptibility, with familial clustering of cardiovascular risk factors amplifying the likelihood of disease manifestation.
9. Poor Diet: Diets rich in saturated fats, trans fats, refined carbohydrates, and excess sodium promote dyslipidemia, hypertension, and endothelial dysfunction, fueling atherosclerosis progression.
9 .Stress: Chronic stress triggers sympathetic nervous system activation and cortisol release, contributing to hypertension, inflammation, and atherosclerosis development
10. Sleep Apnea: Obstructive sleep apnea, characterized by recurrent episodes of upper airway obstruction during sleep, disrupts normal cardiovascular function and exacerbates atherosclerosis progression.
Identifying and addressing these risk factors through targeted interventions and lifestyle modifications are essential for mitigating the burden of atherosclerosis and reducing the risk of cardiovascular events.
Diagnosis and Treatment of Atherosclerosis

Accurate diagnosis and effective management of atherosclerosis require a multidisciplinary approach involving clinical evaluation, imaging studies, and laboratory testing. Diagnostic modalities utilized in the assessment of atherosclerosis include:
Physical Examination: Healthcare providers perform a comprehensive physical examination, assessing vital signs, auscultating for abnormal heart sounds or bruits, and palpating for peripheral pulses to evaluate cardiovascular health.
Imaging Tests: Various imaging modalities are employed to visualize arterial anatomy, assess plaque burden, and identify areas of stenosis or occlusion. These includes;
Angiography: Intravascular contrast dye is utilized to visualize arterial lumens and detect areas of stenosis or occlusion via X-ray imaging.
Ultrasound: Non-invasive ultrasound techniques, such as carotid ultrasound or abdominal ultrasound, enable the assessment of arterial wall thickness, plaque morphology, and blood flow characteristics.
Computed Tomography (CT) Angiography: CT angiography provides detailed anatomical imaging of arterial structures, facilitating the identification of atherosclerotic lesions and assessing their severity.
Magnetic Resonance Angiography (MRA): MRA employs magnetic resonance imaging (MRI) techniques to generate high-resolution images of blood vessels, aiding in the evaluation of arterial stenosis, plaque composition, and hemodynamic parameters.
3. Laboratory Evaluations: Blood tests are conducted to assess lipid profiles, inflammatory markers, and other biochemical parameters associated with cardiovascular risk. These include
Lipid Profile: Measurement of serum lipid levels, including total cholesterol, LDL cholesterol, high-density lipoprotein (HDL) cholesterol, and triglycerides, provides insight into atherosclerosis risk and treatment efficacy.
Inflammatory Markers: Assessment of inflammatory biomarkers, such as C-reactive protein (CRP) or interleukin-6 (IL-6), aids in risk stratification and monitoring disease activity in individuals with atherosclerosis.
Blood Glucose: Screening for abnormal glucose metabolism, including fasting blood glucose and hemoglobin A1c (HbA1c) levels, helps identify individuals at risk of diabetes-associated atherosclerosis complications
4. Functional Tests: Functional assessments, such as stress testing or ankle-brachial index (ABI) measurement, are performed to evaluate cardiovascular function and assess the impact of atherosclerosis on tissue perfusion.
Once diagnosed, the management of atherosclerosis encompasses various approach targeting risk factor modification, pharmacological intervention, and, when indicated, invasive procedures to alleviate arterial obstruction and prevent cardiovascular events.
Treatment strategies for atherosclerosis include:
Lifestyle Modifications: Lifestyle interventions form the cornerstone of atherosclerosis management, emphasizing dietary modifications, regular physical activity, smoking cessation, stress reduction, and weight management to optimize cardiovascular health and mitigate disease progression.
Medication Management: Pharmacological therapy plays a pivotal role in atherosclerosis treatment, targeting modifiable risk factors such as dyslipidemia, hypertension, and inflammation. Commonly prescribed medications include
Statins: HMG-CoA reductase inhibitors, such as atorvastatin or simvastatin, reduce LDL cholesterol levels and stabilize atherosclerotic plaques, lowering the risk of cardiovascular events.
Antihypertensive Agents: Angiotensin-converting enzyme (ACE) inhibitors, angiotensin II receptor blockers (ARBs), beta-blockers, and calcium channel blockers are utilized to control blood pressure and mitigate endothelial dysfunction in individuals with hypertension-associated atherosclerosis.
Antiplatelet Therapy: Aspirin and other antiplatelet agents, such as clopidogrel or ticagrelor, inhibit platelet aggregation and reduce the risk of thrombotic events in individuals with established atherosclerosis or high cardiovascular risk.
Antidiabetic Medications: Oral hypoglycemic agents, insulin, or glucagon-like peptide-1 (GLP-1) receptor agonists are prescribed to achieve glycemic control and minimize the risk of diabetes-related atherosclerosis complications.
3. Invasive Procedures: In cases of severe arterial stenosis or symptomatic atherosclerotic disease refractory to medical therapy, invasive interventions may be warranted to restore arterial patency and alleviate ischemic symptoms. These include:
Percutaneous Coronary Intervention (PCI): Angioplasty with or without stent placement is performed to widen narrowed coronary arteries and improve myocardial perfusion in individuals with coronary artery disease (CAD).
Coronary Artery Bypass Grafting (CABG): Surgical revascularization using autologous or synthetic conduits bypasses obstructed coronary vessels, restoring blood flow to ischemic myocardial territories in patients with multivessel CAD or left main coronary artery disease.
Carotid Endarterectomy: Surgical removal of atherosclerotic plaque from carotid arteries reduces the risk of stroke in individuals with significant carotid stenosis and a history of transient ischemic attacks (TIAs) or cerebrovascular events.
Peripheral Arterial Interventions: Endovascular procedures, such as angioplasty, stenting, or atherectomy, are performed to treat lower extremity arterial disease and alleviate claudication symptoms in patients with peripheral artery disease (PAD).
Secondary Prevention Strategies: Beyond acute management, secondary prevention measures aim to prevent recurrent cardiovascular events and minimize disease progression through comprehensive risk factor modification, medication adherence, and ongoing surveillance of disease activity
Prevention of Atherosclerosis

Preventive strategies for atherosclerosis focus on addressing modifiable risk factors and promoting cardiovascular health through lifestyle modifications, health education, and targeted interventions. Key components of atherosclerosis prevention include:
Healthy Lifestyle: Encouraging individuals to adopt a healthy lifestyle characterized by balanced nutrition, regular physical activity, adequate sleep, stress management, and avoidance of harmful habits such as smoking or excessive alcohol consumption is paramount for reducing atherosclerosis risk
2. Dietary Modifications: Emphasizing a heart-healthy diet rich in fruits, vegetables, whole grains, lean proteins, and unsaturated fats while limiting intake of saturated fats, trans fats, cholesterol, sodium, and added sugars helps optimize lipid profiles, blood pressure, and overall cardiovascular health.
3. Physical Activity: Promoting regular exercise and physical activity is essential for maintaining cardiovascular fitness, weight management, insulin sensitivity, and endothelial function, thereby reducing the risk of atherosclerosis and its complications.
4. Tobacco Cessation: Implementing tobacco cessation programs and providing support for smoking cessation initiatives are critical for reducing atherosclerosis risk and improving overall cardiovascular outcomes.
5. Stress Management: Teaching stress reduction techniques such as mindfulness meditation, yoga, deep breathing exercises, or cognitive-behavioral therapy empowers individuals to cope with stressors effectively and mitigate their detrimental effects on cardiovascular health.
5 . Health Education: Educating individuals about the risks associated with atherosclerosis, the importance of early detection, and the benefits of preventive measures fosters informed decision-making and empowers individuals to take proactive steps towards cardiovascular wellness.
6. Regular Screening: Encouraging regular medical checkups and health screenings enables early detection of cardiovascular risk factors, facilitating timely intervention and personalized risk stratification for individuals at heightened risk of atherosclerosis.
Conclusion
In conclusion, atherosclerosis represents a significant public health challenge with far-reaching implications for cardiovascular morbidity and mortality. By majoring on the pathophysiology of atherosclerosis, identifying modifiable risk factors, and implementing evidence-based preventive strategies, healthcare providers can effectively mitigate the burden of atherosclerotic disease and promote cardiovascular health across diverse populations. Empowering individuals with knowledge, facilitating lifestyle modifications, and fostering a collaborative approach to atherosclerosis prevention and management are essential steps towards achieving optimal cardiovascular outcomes and enhancing quality of life for individuals affected by this pervasive condition.
As you navigate the complexities of cardiovascular health, remember that support and guidance are always available. Seek assistance from Expert Academic Assignment Help whenever needed.
Your journey in medicine is about more than just acquiring knowledge — it’s about embodying compassion, empathy, and continuous learning. Together, let’s strive for optimal cardiovascular health for all.
Email us at expertassignment46@gmail.com
Wishing you success and fulfillment in your medical journey.
Cerebral Palsy

Introduction
Cerebral palsy (CP) is not only a neurological condition but also a lifelong journey for individuals and their families. The impacts of CP extend far beyond physical limitations, encompassing social, emotional, and economic aspects. Understanding the complexities of CP is crucial for healthcare professionals, educators, policymakers, and society at large to provide adequate support and resources for affected individuals.
In recent years, there has been a growing recognition of the diversity within the CP community, with an emphasis on individualized care and inclusive practices. By fostering a deeper understanding of CP, we can promote empowerment, advocacy, and meaningful participation for individuals with CP in all aspects of life.
Symptoms and Types

The symptoms of CP can manifest in various ways, depending on the severity and type of the condition. For some individuals, muscle stiffness or spasticity may be the predominant feature, leading to difficulties in movement and coordination. Others may experience involuntary movements or dyskinetic movements, characterized by writhing or twisting motions. Mixed types of CP present with a combination of spastic and dyskinetic features, further complicating the clinical picture.
In addition to motor impairments, individuals with CP may also experience associated conditions such as intellectual disability, epilepsy, communication difficulties, and sensory impairments. These coexisting conditions can significantly impact the daily lives of affected individuals and require comprehensive management strategies tailored to their unique needs.
Causes and Risk Factors

Prenatal factors such as premature birth, low birth weight, maternal infections, and genetic abnormalities play a significant role in the development of CP. Maternal health conditions like preeclampsia and gestational diabetes may also increase the risk of CP, highlighting the importance of maternal health during pregnancy.
Perinatal events such as birth asphyxia, neonatal stroke, or brain hemorrhage can result in brain injury and subsequent CP. Postnatal factors such as traumatic brain injury, infections, or accidents can also contribute to the development of CP, underscoring the need for vigilance and prompt intervention in the neonatal period and beyond.
Certain maternal and environmental factors, including multiple pregnancies, maternal substance use, and advanced maternal age, may further predispose individuals to CP. Addressing these modifiable risk factors through public health initiatives, prenatal care, and early intervention programs is essential for reducing the burden of CP on affected individuals and their families.
Diagnosis and Management

The diagnosis of CP is often made based on clinical assessment and observation of motor impairments, developmental delays, and associated conditions. Medical history, including prenatal, perinatal, and postnatal factors, provides valuable insights into potential risk factors and contributing factors for CP. Developmental assessments, such as the Denver Developmental Screening Test or the Bayley Scales of Infant and Toddler Development, can help identify delays in reaching developmental milestones and guide early intervention strategies.
Physical examination plays a critical role in evaluating muscle tone, reflexes, coordination, and posture. Neuroimaging studies, including magnetic resonance imaging (MRI) and computed tomography (CT) scans, may reveal structural abnormalities or lesions in the brain indicative of CP. These diagnostic tools help healthcare professionals confirm the diagnosis of CP and tailor management strategies to address the specific needs of affected individuals.
Early intervention is paramount in optimizing outcomes for individuals with CP, as neuroplasticity is greatest during the early years of life. A multidisciplinary approach involving healthcare professionals from various disciplines, including pediatricians, neurologists, physiatrists, physical therapists, occupational therapists, speech therapists, and social workers, ensures comprehensive care and support for affected individuals and their families.
Management strategies for CP encompass a range of interventions aimed at addressing motor impairments, enhancing functional abilities, and promoting independence. Medical interventions may include medications to manage symptoms such as spasticity, seizures, or associated conditions. Physical therapy focuses on improving mobility, strength, and coordination through exercises, stretches, and functional activities. Occupational therapy helps individuals develop skills for activities of daily living, such as feeding, dressing, and grooming. Speech therapy addresses communication difficulties and swallowing disorders, enhancing oral motor skills and facilitating effective communication. Orthotic devices, such as braces or splints, may be prescribed to improve posture, stability, and mobility. Assistive technology, including communication devices, mobility aids, and adaptive equipment, can enhance independence and quality of life for individuals with CP. Surgical interventions, such as selective dorsal rhizotomy or orthopedic procedures, may be considered to reduce spasticity, correct musculoskeletal deformities, or improve functional outcomes.
The management of CP is highly individualized, with treatment plans tailored to address the specific needs and goals of each individual. Regular follow-up visits with healthcare providers allow for ongoing assessment, monitoring, and adjustment of management strategies as needed. Family-centered care, collaboration between healthcare professionals, educators, and community resources, and advocacy for inclusive practices are essential in supporting individuals with CP and promoting their overall well-being.
Prognosis and Living With CP

The prognosis for individuals with CP varies widely depending on various factors, including the severity and type of CP, the presence of associated conditions, access to medical care and supportive services, and individual factors such as resilience, motivation, and social support. While some individuals may experience significant functional limitations and require lifelong assistance, others may achieve remarkable milestones and lead independent lives.
Advances in medical care, including early intervention programs, multidisciplinary care teams, and innovative treatment modalities, have contributed to improved outcomes and quality of life for individuals with CP. Early identification and intervention, coupled with ongoing support and rehabilitation services, play a crucial role in optimizing functional outcomes and promoting independence.
Living with CP requires resilience, perseverance, and adaptation to overcome physical, emotional, and social challenges. Individuals with CP may face barriers to participation in education, employment, and social activities due to mobility limitations, communication difficulties, and societal attitudes toward disability. Advocacy efforts, disability rights initiatives, and inclusive policies are essential in promoting equal opportunities, accessibility, and social inclusion for individuals with CP.
Family support, peer networks, and community resources play a vital role in providing emotional support, practical assistance, and social connections for individuals with CP and their families. Building resilience, fostering independence, and nurturing self-esteem are essential in empowering individuals with CP to advocate for their needs, pursue their goals, and lead fulfilling lives.
Conclusion
Cerebral palsy is a complex neurological disorder that requires a comprehensive understanding and multidisciplinary approach to diagnosis, management, and support. By addressing the diverse needs of affected individuals and their families, fostering inclusive practices, and advocating for equal opportunities, we can promote the well-being and full participation of individuals with CP in society. Continued research, education, and advocacy are essential in advancing our understanding of CP, improving outcomes, and enhancing the quality of life for affected individuals and their families
Remember, success in your academic endeavors is within reach. Whether you’re facing challenges or seeking to elevate your performance, don’t hesitate to reach out for expert guidance and support. I’m here to assist you every step of the way. Reach me at williamsassignmenthelpfredrick@gmail.com
Let’s embark on this journey towards academic excellence together. Looking forward to hearing from you soon.
Cervical Cancer

Introduction
Cervical cancer is a significant health concern affecting women worldwide. It arises from abnormal cell growth in the cervix, often linked to the human papillomavirus (HPV). Despite advancements in prevention and treatment, cervical cancer remains a leading cause of cancer-related deaths among women. Understanding its causes, symptoms, risk factors, and prevention strategies is crucial for early detection and effective management.
1. Understanding Cervical Cancer

Cervical cancer originates in the cervix, the lower part of the uterus connecting to the vagina.
HPV, a common sexually transmitted infection, is a primary cause of cervical cancer, with certain strains posing higher risks.
The body’s immune response typically clears HPV infections, but persistent infections can lead to cervical cell abnormalities and eventually cancer.
2. Symptoms and Diagnosis

Cervical cancer may not present noticeable symptoms initially, making regular screenings essential for early detection.
Symptoms can include abnormal vaginal bleeding, pelvic pain, and unusual discharge.
Diagnostic methods include Pap tests, HPV DNA testing, colposcopy, and biopsy to confirm cervical cancer and determine its stage.
3. Treatment Options

Treatment depends on the cancer’s stage, size, and type, as well as the patient’s overall health and preferences.
Surgical interventions, such as hysterectomy or removal of cancerous tissue, are common for early-stage cervical cancer.
Advanced stages may require a combination of surgery, chemotherapy, radiation therapy, or targeted therapy to eliminate cancer cells and prevent recurrence.
4. Risk Factors and Prevention
Several factors increase the risk of developing cervical cancer, including HPV infection, smoking, early sexual activity, and weakened immune system.
Prevention strategies include HPV vaccination, routine Pap tests for early detection of precancerous lesions, practicing safe sex, and smoking cessation.
5. Impact on Women’s Health

Cervical cancer not only affects physical health but also has emotional, social, and financial repercussions on women and their families.
Access to screening, vaccination, and treatment services significantly impacts the prognosis and survival rates of women diagnosed with cervical cancer.
Addressing disparities in healthcare access and promoting awareness about cervical cancer prevention are crucial for improving women’s health outcomes globally.
Conclusion
Cervical cancer remains a significant public health challenge despite advancements in prevention and treatment. Early detection through regular screenings and vaccination against HPV can significantly reduce the burden of this disease. Moreover, addressing risk factors such as smoking and promoting safe sexual practices are vital for cervical cancer prevention. By raising awareness, improving access to healthcare services, and advocating for comprehensive cervical cancer prevention programs, we can strive towards reducing the incidence and mortality associated with this preventable disease, ultimately enhancing women’s health and well-being worldwide.
We wish you all the best in your medical education journey. In case you need any guidance or assistance during the learning process, do not hesitate to reach out to us.
Email at;
williamsassignmenthelpfredrick@gmail.com
Your Digestive System & How it Works

Introduction
The digestive system is a marvel of biological process that involves the breakdown of food into absorbable nutrients essential for sustaining life. Comprising a network of organs and tissues, it serves as the body’s processing center, converting ingested substances into energy, growth materials, and waste. Understanding the intricacies of this system provides profound insights into human physiology and health maintenance.
1. Anatomy of the Digestive System

The digestive system is a complex network of organs, glands, and tissues that work in harmony to facilitate the digestion and absorption of nutrients. At its core lies the gastrointestinal tract (GI tract), a continuous tube extending from the mouth to the anus. Key components of the GI tract include the mouth, esophagus, stomach, small intestine, large intestine, and anus. Additionally, accessory organs such as the liver, pancreas, and gallbladder contribute crucial digestive enzymes and fluids to aid in the breakdown of food.
2. Functions of the Digestive System

The primary function of the digestive system is to process food and liquids to extract essential nutrients while eliminating waste products. Through a series of coordinated processes, including ingestion, digestion, absorption, and excretion, the digestive system ensures the body receives the necessary components for energy production, tissue repair, and growth. Moreover, it plays a vital role in maintaining fluid and electrolyte balance within the body.
3. Digestive process

Digestion begins in the mouth, where mechanical and chemical processes break down food into smaller particles. Chewing, or mastication, mechanically reduces food size, while saliva, secreted by salivary glands, initiates the chemical breakdown of carbohydrates through the action of enzymes like amylase. The bolus of food then travels down the esophagus via peristaltic contractions, entering the stomach for further processing.
In the stomach, gastric juices containing hydrochloric acid and pepsin begin the breakdown of proteins, while muscular contractions churn the food into a semi-liquid mixture known as chyme. From the stomach, chyme enters the small intestine, where the majority of nutrient absorption occurs. Enzymes from the pancreas and bile from the liver aid in the breakdown of fats, proteins, and carbohydrates, allowing for absorption across the intestinal lining.
In the large intestine, water absorption occurs, leading to the formation of feces. Microbial fermentation within the colon further breaks down indigestible carbohydrates and produces essential nutrients like vitamin K and certain B vitamins. Finally, waste products are expelled through the anus during defecation.
4. Regulation of Digestive Processes

The intricate processes of digestion are tightly regulated by a combination of neural, hormonal, and local mechanisms. Neural signals originating from the brain and enteric nervous system (ENS) coordinate muscle contractions along the GI tract, ensuring the smooth passage of food and efficient mixing with digestive juices. Hormones such as gastrin, secretin, and cholecystokinin act as chemical messengers, modulating gastric acid secretion, pancreatic enzyme release, and bile production in response to dietary stimuli.
5. Clinical Implications and Disorders

Disruptions to the normal functioning of the digestive system can lead to a myriad of health disorders, ranging from minor discomforts to life-threatening conditions. Gastrointestinal disorders encompass a broad spectrum of diseases, including gastroesophageal reflux disease (GERD), peptic ulcers, inflammatory bowel disease (IBD), and colorectal cancer. These conditions often manifest with symptoms such as abdominal pain, bloating, diarrhea, constipation, and rectal bleeding, necessitating thorough diagnostic evaluation and tailored treatment approaches.
6. Research and Advancements

Advancements in medical research continue to deepen our understanding of digestive physiology and pathology, paving the way for innovative diagnostic techniques and therapeutic interventions. Clinical trials conducted by academic institutions and pharmaceutical companies play a pivotal role in evaluating novel treatment modalities and improving patient outcomes. Areas of active investigation include microbiome research, targeted drug delivery systems, and minimally invasive surgical techniques for gastrointestinal disorders.
Conclusion
In conclusion, the digestive system serves as a cornerstone of human biology, enabling the breakdown and assimilation of nutrients essential for life. Its intricate anatomy and physiological processes underscore the remarkable complexity of the human body. By elucidating the mechanisms of digestion and exploring the clinical implications of digestive disorders, we gain valuable insights into the maintenance of health and the management of disease. Continued research efforts hold the promise of further enhancing our understanding and treatment of gastrointestinal conditions, ultimately improving the quality of life for individuals worldwide.
We wish you all the best in your medical education journey. In case you need any guidance or assistance during the learning process, do not hesitate to reach out to us.
Email at;
williamsassignmenthelpfredrick@gmail.com
Brain Tumor

Introduction
Brain tumors represent a complex and diverse group of neoplasms that arise from abnormal growth of cells within the brain or its surrounding structures. These tumors can vary widely in terms of their location, size, aggressiveness, and clinical presentation. Understanding the intricacies of brain tumors, including their diagnosis, treatment, and prognosis, requires a comprehensive approach that integrates medical expertise, advanced imaging modalities, and personalized therapeutic interventions.
Diagnosis of Brain Tumor

The diagnosis of a brain tumor typically begins with a thorough clinical evaluation, including a detailed medical history and neurological examination. Symptoms suggestive of a brain tumor may include persistent headaches, seizures, cognitive deficits, changes in behavior or personality, and focal neurological deficits such as weakness or sensory disturbances. However, it’s essential to recognize that many of these symptoms are nonspecific and can be caused by various other conditions.
To confirm the presence of a brain tumor and characterize its specific features, a variety of imaging studies and laboratory tests may be employed. These include computed tomography (CT) scans, magnetic resonance imaging (MRI), and positron emission tomography (PET) scans. CT scans provide detailed cross-sectional images of the brain and are often the initial imaging modality used to assess patients with suspected brain tumors due to their widespread availability and rapid results. MRI, on the other hand, offers superior soft tissue contrast and is particularly useful for delineating the precise location and extent of brain tumors. In some cases, contrast-enhanced MRI with gadolinium-based contrast agents may be performed to enhance visualization of tumor tissue and surrounding structures.
Advanced MRI techniques, such as functional MRI (fMRI), magnetic resonance spectroscopy (MRS), and perfusion-weighted imaging (PWI), can provide additional information about the functional characteristics and metabolic activity of brain tumors. These modalities play a crucial role in treatment planning and assessing tumor response to therapy.
In select cases, a PET scan may be utilized to evaluate the metabolic activity of brain tumors and differentiate between benign and malignant lesions. PET imaging with radiopharmaceutical tracers such as fluorodeoxyglucose (FDG) can help identify areas of increased glucose metabolism, which are typically indicative of rapidly growing tumor cells. Additionally, molecular imaging techniques targeting specific biomarkers may offer insights into the molecular profile and biological behavior of brain tumors, facilitating personalized treatment strategies.
Tissue Sampling and Histopathological Evaluation: While imaging studies provide valuable information about the radiographic characteristics of brain tumors, definitive diagnosis often requires histopathological analysis of tissue samples obtained via biopsy or surgical resection. Tissue sampling allows for detailed microscopic examination of tumor cells, assessment of histological features, and determination of tumor grade, which plays a crucial role in prognostication and treatment planning.
Brain tumor grading is based on the World Health Organization (WHO) classification system, which stratifies tumors into different grades (I-IV) based on their histological features and biological behavior. Grade I tumors are typically slow-growing and well-differentiated, while grade IV tumors are highly aggressive and rapidly proliferating. Intermediate grades (II-III) exhibit varying degrees of aggressiveness and cellular atypia.
Prognostic Factors and Treatment Consideration

The prognosis of patients with brain tumors is influenced by various factors, including tumor type, grade, location, extent of resection, molecular characteristics, and patient-specific factors such as age and overall health status. High-grade tumors, such as glioblastoma multiforme, are associated with poorer outcomes compared to low-grade tumors, necessitating more aggressive treatment approaches.
Treatment strategies for brain tumors are highly individualized and may encompass a combination of surgical resection, radiation therapy, chemotherapy, targeted therapy, and supportive care measures. The goals of treatment are to achieve maximal tumor control while preserving neurological function and quality of life. Surgical resection is often the initial step in the management of operable brain tumors, with the aim of achieving gross total resection whenever feasible. However, the proximity of tumors to critical brain structures and eloquent areas may limit the extent of surgical resection and necessitate adjuvant therapies.
Surgical Management of Brain Tumor

Surgical approaches to brain tumor resection have evolved significantly with advances in neuroimaging, neurosurgical techniques, and intraoperative navigation systems. Traditional open craniotomy remains the standard approach for many brain tumors, allowing for direct access to the intracranial lesion. Microsurgical techniques, including the use of operating microscopes and intraoperative neuro navigation systems, enable precise tumor localization and maximal safe resection while minimizing damage to adjacent healthy brain tissue.
In recent years, minimally invasive approaches such as endoscopic endonasal surgery and keyhole craniotomy have gained popularity for select brain tumors, offering advantages such as smaller incisions, reduced surgical morbidity, and faster recovery times. Endoscopic techniques, in particular, allow for access to deep-seated lesions through natural orifices, such as the nasal cavity, thereby avoiding the need for extensive craniotomies and brain retraction.
Radiation Therapy for Brain Tumors

Radiation therapy plays a critical role in the management of both primary and metastatic brain tumors, offering precise and localized delivery of ionizing radiation to target tumor cells while sparing adjacent normal brain tissue. External beam radiation therapy (EBRT) is the most commonly utilized modality, utilizing high-energy X-rays or protons to deliver radiation to the tumor site over multiple treatment sessions. Techniques such as intensity-modulated radiation therapy (IMRT) and stereotactic radiosurgery (SRS) allow for highly conformal dose delivery, enabling escalation of radiation doses to the tumor while minimizing toxicity to surrounding critical structures.
In addition to conventional EBRT, brachytherapy techniques may be employed for selected cases, involving the placement of radioactive sources directly into or adjacent to the tumor cavity during surgical resection. This allows for localized delivery of high-dose radiation while minimizing exposure to healthy tissues. Proton therapy, a form of particle therapy, offers the advantage of improved dose conformity and reduced integral dose to surrounding tissues compared to conventional photon-based radiation therapy. Proton therapy is particularly beneficial for treating pediatric brain tumors and tumors located near critical structures, such as the optic nerves and brainstem.
Chemotherapy and Targeted Therapy: Chemotherapy plays a crucial role in the management of certain brain tumors, particularly high-grade gliomas and metastatic lesions. Chemotherapeutic agents may be administered orally, intravenously, or intracranially, either as monotherapy or in combination with other treatment modalities. The choice of chemotherapy regimen depends on factors such as tumor type, molecular characteristics, and patient-specific considerations.
Targeted therapy has emerged as a promising treatment approach for select brain tumors, leveraging the identification of specific molecular targets or pathways implicated in tumor growth and progression. Targeted agents may include small molecule inhibitors, monoclonal antibodies, or immunotherapeutic agents designed to selectively target tumor cells while sparing normal tissues. Biomarker-driven approaches, such as molecular profiling and genetic testing, help identify patients who are most likely to benefit from targeted therapies, enabling a personalized approach to treatment selection.
Recovery and Rehabilitation

Recovery following treatment for brain tumors often requires comprehensive rehabilitation efforts aimed at optimizing functional outcomes and quality of life. Physical therapy, occupational therapy, speech therapy, and cognitive rehabilitation play important roles in addressing deficits related to motor function, activities of daily living, communication, and cognition. Additionally, psychosocial support services and caregiver education are essential components of the multidisciplinary care team, providing emotional support and practical assistance to patients and their families throughout the treatment and recovery process.
Conclusion
In conclusion, the management of brain tumors necessitates a multidisciplinary and individualized approach that integrates advances in diagnostic imaging, surgical techniques, radiation therapy, chemotherapy, targeted therapy, and supportive care interventions. Collaborative decision-making between patients, healthcare providers, and allied health professionals is paramount in optimizing treatment outcomes and enhancing quality of life for individuals affected by brain tumors. Ongoing research efforts aimed at elucidating the molecular mechanisms underlying tumorigenesis, identifying novel therapeutic targets, and refining treatment strategies offer hope for continued advancements in the field of neuro-oncology and improved outcomes for patients with brain tumors.
We wish you all the best in your medical education journey. In case you need any guidance or assistance during the learning process, do not hesitate to reach out to us.
Email at;
williamsassignmenthelpfredrick@gmail.com
10 Common Dental Problems

Introduction
Maintaining optimal dental health is crucial not only for a winning smile but also for overall well-being. However, numerous individuals encounter common dental issues that can affect their quality of life. From tooth decay to gum disease, understanding these problems and their treatments is essential for preventing complications and preserving oral health. This comprehensive guide explores ten prevalent dental problems and outlines effective treatment options for each, empowering individuals to make informed decisions about their dental care.
1.Tooth Decay

Tooth decay, also known as dental caries, is a pervasive dental issue caused by the accumulation of plaque and the subsequent erosion of tooth enamel. This section delves into the causes, symptoms, and treatment options for tooth decay, emphasizing the importance of preventive measures such as regular brushing, flossing, and dental check-ups.
2. Gum Disease

Gingivitis and periodontitis are two stages of gum disease characterized by inflammation and bacterial infection of the gums. Exploring the risk factors, symptoms, and management strategies for gum disease sheds light on the importance of proper oral hygiene practices and professional dental interventions in preserving gum health.
3.Bad Breath

Halitosis, or bad breath, can stem from various underlying factors such as poor oral hygiene, dry mouth, and underlying medical conditions. This segment examines the causes of bad breath and highlights the significance of comprehensive dental assessments and tailored treatment plans to address this common concern effectively.
4.Sensitive Teeth

Tooth sensitivity, characterized by discomfort in response to hot, cold, or sweet stimuli, often results from enamel erosion or underlying dental issues. Delving into the potential causes and management options for sensitive teeth underscores the role of personalized dental care in alleviating discomfort and enhancing oral comfort.
5.Cracked or Broken Teeth

Cracks or fractures in teeth can result from trauma, bruxism (teeth grinding), or other factors, leading to pain and functional impairment. This section explores the diagnostic procedures and treatment modalities available for repairing cracked or broken teeth, emphasizing the importance of prompt intervention to prevent further damage.
6.Receding Gums

Receding gums, characterized by the exposure of tooth roots due to gum tissue loss, can result from various factors, including poor oral hygiene and genetic predispositions. Analyzing the causes, consequences, and treatment approaches for receding gums underscores the significance of preventive measures and professional interventions in preserving gum health.
7. Root Infection

Root infections, often resulting from untreated cavities or trauma, can lead to severe pain and dental abscesses if left untreated. This segment elucidates the diagnostic techniques and treatment options for root infections, highlighting the role of root canal therapy in alleviating symptoms and preserving tooth structure.
8. Enamel Erosion

Enamel erosion, characterized by the gradual loss of tooth enamel due to acidic and sugary dietary habits, poses significant challenges to dental health. Exploring preventive strategies and restorative treatments for enamel erosion underscores the importance of dietary modifications and proactive dental care in preserving tooth structure and function.
9. Dry Mouth

Xerostomia, or dry mouth, can result from various factors, including medication side effects and underlying medical conditions. This section examines the causes, symptoms, and management strategies for dry mouth, emphasizing the importance of hydration and lifestyle modifications in alleviating discomfort and preventing oral complications.
10. Teeth Grinding
Bruxism, characterized by involuntary teeth grinding or clenching, can lead to tooth wear, jaw pain, and headaches. Exploring the underlying causes and treatment options for bruxism underscores the importance of stress management and protective dental appliances in mitigating symptoms and preserving dental health.
Conclusion
In conclusion, understanding and addressing common dental problems are essential steps toward maintaining optimal oral health and overall well-being. By recognizing the signs and symptoms of tooth decay, gum disease, and other dental issues, individuals can seek timely intervention and preventive care to mitigate risks and preserve their smiles. Through a combination of proper oral hygiene practices, regular dental check-ups, and personalized treatment plans, individuals can navigate common dental challenges with confidence and achieve lasting oral health. Embracing proactive dental care and seeking professional assistance when needed are crucial components of a comprehensive approach to dental wellness.
In exploring and pursuing your dental studies, we wish you all the best in becoming a dentist. In case you encounter challenges or need guidance during this study period, do not hesitate to contact us.
Email at;williamsassignmenthelpfredrick@gmail.com
Breast Cancer

Introduction
Breast cancer, a multifaceted and prevalent disease, poses a significant health challenge globally, transcending gender lines with its potential impact. Characterized by the abnormal proliferation of cells within breast tissue, breast cancer’s complex etiology remains an area of intense study and concern. Despite notable advancements in medical science and increased awareness, it continues to be a leading cause of morbidity and mortality worldwide. This comprehensive discussion aims to delve into the intricacies of breast cancer, encompassing its causes, risk factors, prevention strategies, diagnostic modalities, treatment options, and the evolving landscape of supportive care.
Causes and Risk Factors

Understanding the underlying causes and risk factors associated with breast cancer is paramount in developing effective prevention and management strategies. While the precise etiology of breast cancer remains elusive, various genetic, hormonal, environmental, and lifestyle factors contribute to its onset and progression. Genetic predispositions, such as mutations in the BRCA1 and BRCA2 genes, significantly elevate the risk of developing breast cancer. Additionally, hormonal influences, including early onset of menstruation, late menopause, and hormone replacement therapy, play a crucial role in disease pathogenesis. Lifestyle factors such as excessive alcohol consumption, obesity, lack of physical activity, and exposure to environmental carcinogens further augment the risk profile.
Preventive Measures

Empowering individuals with knowledge about preventive measures is essential in mitigating the burden of breast cancer. Promoting regular breast self-examinations, clinical breast examinations, and mammographic screenings facilitates early detection and intervention. Emphasizing lifestyle modifications, including maintaining a healthy weight, adopting a balanced diet rich in fruits and vegetables, limiting alcohol intake, and engaging in regular physical activity, can reduce the risk of breast cancer. For individuals with a heightened risk due to genetic predispositions or familial history, prophylactic surgeries, such as mastectomy or oophorectomy, and chemo preventive agents offer viable preventive options.
Diagnostic Modalities

Advances in diagnostic modalities have revolutionized the early detection and diagnosis of breast cancer, enabling prompt initiation of treatment and improved clinical outcomes. Mammography remains the cornerstone of breast cancer screening, capable of detecting abnormalities such as microcalcifications, masses, or architectural distortions. Complementary imaging techniques, including ultrasound, magnetic resonance imaging (MRI), and molecular breast imaging (MBI), enhance diagnostic accuracy, particularly in women with dense breast tissue or high-risk profiles. Biopsy procedures, such as core needle biopsy or surgical excision, facilitate histopathological examination, enabling precise diagnosis and classification of breast lesions.
Treatment Options

Tailoring treatment strategies to individual patient characteristics and disease parameters is essential in optimizing therapeutic outcomes in breast cancer. The treatment landscape encompasses a multidisciplinary approach, integrating surgical, medical, and radiation oncology interventions. Surgical options range from breast-conserving surgeries, such as lumpectomy or segmental mastectomy, to radical procedures like total mastectomy or modified radical mastectomy, depending on tumor size, location, and extent of spread. Adjuvant therapies, including chemotherapy, hormonal therapy, targeted therapy, and immunotherapy, aim to eradicate residual disease, prevent recurrence, and improve overall survival. Radiation therapy, administered either postoperatively or as a primary modality in selected cases, targets residual tumor cells, minimizing locoregional recurrence rates.
Supportive Care and Survivorship

Recognizing the holistic needs of breast cancer patients and survivors is integral in promoting comprehensive care and ensuring optimal quality of life. Supportive care interventions, including symptom management, psychosocial support, nutritional counseling, and rehabilitation services, address the multifaceted challenges associated with cancer diagnosis and treatment. Survivorship programs, focusing on survivorship care planning, surveillance for recurrence, long-term monitoring of treatment-related complications, and health promotion initiatives, facilitate the transition from active treatment to survivorship. Engaging patients and caregivers in survivorship care planning fosters empowerment, resilience, and a sense of agency in navigating the post-treatment phase.
Conclusion
In conclusion, breast cancer represents a formidable health challenge with profound implications for affected individuals, families, and communities worldwide. While significant strides have been made in understanding its pathophysiology, enhancing diagnostic capabilities, and expanding treatment options, concerted efforts are warranted to address existing gaps in prevention, early detection, and access to care. By fostering collaborative partnerships among stakeholders, advocating for evidence-based interventions, and promoting health equity, we can strive towards a future where breast cancer incidence and mortality rates are substantially reduced. Through continued innovation, education, and advocacy, we can transform the landscape of breast cancer care, offering hope, support, and healing to those impacted by this pervasive disease.
We wish you all the best in your medical education journey. In case you need any guidance or assistance during the learning process, do not hesitate to reach out to us.
Email at;
williamsassignmenthelpfredrick@gmail.com
Anatomy of the Heart

Introduction
The heart, an extraordinary organ vital to human life, serves as the epicenter of the circulatory system, tirelessly pumping blood throughout the body. Its intricate anatomy and physiological functions are the focus of extensive study and admiration in medical science. This comprehensive overview aims to delve into the intricate details of the heart’s anatomy, its valves, the circulation of blood within its chambers, and the critical role it plays in sustaining life.
Anatomy of the Heart
The heart, nestled within the middle mediastinum, is encased by a protective serous sac known as the pericardium. Structurally resembling a quadrangular pyramid, its base aligns posteriorly while its apex points anteriorly towards the thoracic wall. The heart’s significance is unparalleled; while one can survive without certain organs, the absence of a heart is incompatible with life.
The heart’s architecture is meticulously organized, with distinct surfaces and margins showing its boundaries. Its internal structure comprises four chambers: two atria and two ventricles. The right atrium and ventricle receive deoxygenated blood from systemic veins and propel it towards the lungs for oxygenation. Conversely, the left atrium and ventricle receive oxygen-rich blood from the lungs and distribute it throughout the body’s systemic vessels.
Heart Valves

Critical to maintaining unidirectional blood flow, the heart is equipped with valves that separate its chambers and prevent backflow. The atrioventricular valves, including the tricuspid and mitral valves, regulate blood flow between atria and ventricles. Semilunar valves, namely the pulmonary and aortic valves, guard the exits of the ventricles, ensuring blood flows into the appropriate vessels without regurgitation.
Blood Flow Through the Heart
The heart’s rhythmic contractions, orchestrated by the cardiac cycle, facilitate the circulation of blood through its chambers. Systole, characterized by ventricular contraction, propels blood into pulmonary and systemic circuits. Diastole, the phase of relaxation, allows chambers to refill with blood. This cyclical process ensures continuous nutrient and oxygen delivery to tissues and organs.
Coronary Circulation

To sustain its relentless activity, the heart receives its own blood supply through the coronary circulation. Coronary arteries originate from the aorta, branching to supply myocardial tissue. Cardiac veins collect deoxygenated blood and converge at the coronary sinus, which empties into the right atrium. This intricate network ensures the heart’s metabolic demands are met, essential for its function.
Great Vessels of the Heart
The great vessels, including the aorta, pulmonary artery, and pulmonary veins, facilitate blood transport to and from the heart. Major branches of the aorta distribute oxygenated blood throughout the body, while the superior and inferior vena cavae return deoxygenated blood from systemic circulation. These vessels play a pivotal role in maintaining systemic homeostasis.
Clinical Insights
Understanding the heart’s anatomy is crucial in diagnosing and managing various cardiac pathologies. Conditions such as angina pectoris, infective endocarditis, and congenital heart diseases underscore the importance of cardiac health. Medical professionals employ diverse interventions, ranging from pharmaceuticals to surgical procedures, to address these conditions and optimize patient outcomes.
In conclusion, the heart’s intricate structure and physiological functions underscore its indispensable role in sustaining life. A deeper comprehension of its anatomy and circulation elucidates the complexities of cardiovascular health and underscores the importance of preventive care and medical intervention in maintaining cardiac well-being.
This overview provides a comprehensive exploration of the heart’s anatomy and functions, offering insights into its pivotal role in human physiology and healthcare.
Best of luck in the strategic study of the heart,
In case you’re experiencing any challenges in the study journey,
Email us at;williamsassignmenthelpfredrick@gmail.com
Medical microbiology


A clinical or medical microbiologist, typically with a Bachelor’s or Master’s degree in Microbiology and sometimes a Ph.D. in life sciences, studies the characteristics of pathogens, their transmission modes, and mechanisms of infection. They play a vital role in providing identification of pathogens, suggesting treatment options, and contributing to the development of health practices.

The historical milestones in medical microbiology include Anton van Leeuwenhoek’s observations of microorganisms in 1676, Edward Jenner’s development of the smallpox vaccine in 1796, and Louis Pasteur’s work on vaccines and pasteurization in 1857. Robert Koch’s germ theory and postulates in the late 19th century were pivotal. The Gram stain, developed by Hans Christian Gram in 1884, revolutionized bacterial identification.

Infectious diseases, including bacterial, viral, parasitic, and fungal, are commonly treated in medical microbiology. Diagnostic tests involve microbial culture, microscopy, biochemical tests, and genotyping. Microbiological culture isolates pathogens in the laboratory, while microscopy provides detailed observations. Biochemical tests and serological methods aid in identifying infectious agents.

However, the rise of antibiotic resistance poses a significant challenge. Medical microbiologists must consider the specificity and effectiveness of antimicrobial drugs, as well as the presence of resistant strains. Phage therapy, an alternative to antibiotics, is being explored to combat antimicrobial resistance.
In conclusion, medical microbiology is a dynamic field that not only diagnoses and treats diseases but also explores the benefits of microbes for human health. With historical milestones and continuous advancements, this field plays a crucial role in shaping healthcare practices and combating infectious diseases.
Wishing you all the best in pursuing your studies in Medical Bacteriology. It involves a lot of detailed focus on the causative agents of diseases.
In case of any challenges or if you’re looking for guidance during the study period, do not hesitate to;
Email us at;williamsassignmenthelpfredrick@mail.com
The pathophysiology of hypertension

Introduction
Hypertension, or high blood pressure, is a complex medical condition affecting a significant proportion of the global population. Despite its prevalence, there remains uncertainty regarding its pathophysiology, with essential hypertension constituting a substantial portion where no single identifiable cause is found. This comprehensive discussion aims to delve into the physiological mechanisms involved in the development of hypertension, exploring factors such as cardiac output, peripheral resistance, the renin-angiotensin-aldosterone system, the autonomic nervous system, endothelial dysfunction, genetic factors, and intrauterine influences.
Cardiac Output and Peripheral Resistance

Maintaining normal blood pressure relies on the delicate balance between cardiac output and peripheral vascular resistance. Essential hypertension often involves a normal cardiac output but elevated peripheral resistance, primarily determined by small arterioles. The role of smooth muscle cells, calcium concentration, and structural changes in arteriolar vessel walls contribute to the irreversible rise in peripheral resistance.
Renin-Angiotensin System

The renin-angiotensin system plays a crucial role in blood pressure regulation. Renin, released in response to various stimuli, initiates the conversion of angiotensinogen to angiotensin I, which is then converted to the vasoconstrictor angiotensin II. This system also stimulates aldosterone release, promoting sodium and water retention. While the circulating system may not be directly responsible for essential hypertension, local renin-angiotensin systems in organs like the kidney, heart, and arterial tree gain significance in regulating regional blood flow.
Autonomic Nervous System

Sympathetic nervous system stimulation affects arteriolar constriction and dilation, playing a pivotal role in maintaining normal blood pressure. Although the exact role of epinephrine and norepinephrine in hypertension etiology remains unclear, drugs blocking the sympathetic nervous system demonstrate therapeutic efficacy.
Endothelial Dysfunction

Vascular endothelial cells, producing vasoactive agents like nitric oxide and endothelin, play a key role in cardiovascular regulation. Endothelial dysfunction, implicated in essential hypertension, involves impaired production of nitric oxide. This dysfunction, once established, becomes irreversible, highlighting its primary nature in hypertension.
Vasoactive Substances

Various vasoactive substances, such as bradykinin, endothelin, atrial natriuretic peptide, and ouabain, influence sodium transport and vascular tone. These substances contribute to the delicate balance in maintaining normal blood pressure.
Genetic Factors
Genetic predisposition significantly contributes to hypertension, with specific mutations linked to disorders like Liddle’s syndrome, glucocorticoid-remediable aldosteronism, and others. The intricate interplay of multiple genes makes it challenging to pinpoint individual contributions.
Intrauterine Influences
Fetal influences, particularly birth weight, emerge as determinants of adult blood pressure. The Barker hypothesis suggests a link between low birth weight, metabolic abnormalities, and hypertension in later life. However, the role of genetic factors in this relationship requires further exploration.
Diastolic Dysfunction

Hypertensive left ventricular hypertrophy leads to impaired diastolic relaxation, affecting ventricular input during exercise. This dysfunction contributes to increased atrial pressure, pulmonary congestion, atrial fibrillation, and potential complications like pulmonary edema.
Conclusion
In conclusion, understanding the pathophysiology of hypertension involves a multifaceted exploration of various physiological mechanisms. While essential hypertension remains a complex and often multifactorial condition, advancements in research shed light on factors such as cardiac output, peripheral resistance, the renin-angiotensin system, the autonomic nervous system, endothelial dysfunction, genetic influences, and intrauterine factors. A comprehensive understanding of these elements is crucial for developing effective therapeutic strategies and preventive measures against the global burden of hypertension.
We hope this helps in improving our comprehension of the Hypertension condition. All the best in your journey in the medical field.
Incase of any challenges' and in need of professional guidance, contact;
Expert Academic Assignment Help at;
williamsassignmenthelpfredrick@gmail.com
Alopecia Areata

Introduction
Alopecia areata is a complex autoimmune disease that targets the body’s hair follicles, resulting in patchy hair loss. While medications and therapies offer hope for regrowth, severe cases may pose challenges in responding to treatment. This comprehensive discussion will delve into the various aspects of alopecia areata, from its symptoms and causes to diagnosis, treatment options, prevention, and the psychosocial impact it can have on individuals.
Symptoms and Causes

Alopecia areata manifests as patchy hair loss on various body parts, commonly affecting the scalp. Understanding its classifications, which include total loss (alopecia areata totalis), full-body hair loss (alopecia areata universalis), diffuse thinning (diffuse alopecia areata), and a band of hair loss (ophiasis alopecia areata), provides insights into the diverse ways it can affect individuals.
Certain factors increase the likelihood of developing alopecia areata, such as being a child, having a family history of the condition, or having autoimmune disorders like diabetes, lupus, or thyroid disease. The prevalence of alopecia areata is significant, with nearly 7 million people in the United States affected, and it is the second-most common form of hair loss.
Psychosocial Impact of Alopecia Areata

Beyond its physical effects, alopecia areata can significantly impact an individual’s psychosocial well-being. The emotional toll of experiencing patchy hair loss, potential nail issues, and the uncertainty of its progression can lead to stress, anxiety, and depression. Recognizing these psychological aspects is crucial for holistic management.
Diagnosis and Tests

Diagnosing alopecia areata involves a thorough examination by healthcare providers, considering medical history, the pattern of hair loss, and familial autoimmune conditions. Additional tests, such as scalp examinations, hair analysis, scalp biopsies, and blood tests, may be conducted to confirm the diagnosis.
Management and Treatment

Managing alopecia areata is a nuanced process, and complete cure remains elusive. Treatment options include corticosteroids, administered through injections, oral pills, or topical applications. Minoxidil (Rogaine®), phototherapy, platelet-rich plasma therapy, and topical immunotherapy are among the diverse approaches employed. The unpredictability of alopecia areata necessitates tailored treatment plans, and response times may vary from weeks to months.
Can Alopecia Areata Go Away?
While alopecia areata itself doesn’t vanish, effective treatments can control hair loss. However, severe forms, such as alopecia areata totalis and alopecia areata universalis, pose greater challenges in treatment response.
Prevention and Outlook

Preventing alopecia areata is currently not feasible. The condition tends to have periods of remission and flare-ups throughout an individual’s life. Outlook varies, with mild cases showing remission and more severe forms being less responsive to available treatments.
Living With Alopecia Areata

Coping with alopecia areata involves adopting various cosmetic and protective measures. These include using makeup to conceal hair loss, wearing coverings like wigs or scarves, and protecting the eyes if eyelashes are affected. A balanced diet and vitamin D supplements may contribute to overall health. Avoiding stress, protecting the skin from the elements, and choosing hair products carefully are essential aspects of self-care.
Conclusion
In conclusion, alopecia areata is a multifaceted condition that extends beyond its physical symptoms. Understanding its classifications, causes, and the psychosocial impact on affected individuals is crucial for comprehensive management. While there is no cure, advancements in treatments offer hope for controlling hair loss and stimulating regrowth. A holistic approach, including psychological support and self-care strategies, empowers individuals to navigate life with alopecia areata confidently. As research progresses, further insights into this autoimmune disorder will likely pave the way for more effective interventions, improving the quality of life for those affected by alopecia areata.
We wish you all the best in your studies and knowledge of Alopecia Disease condition.
In case of any challenges during your studies and education journey, don’t hesitate to contact us for a flawless process.
Email us through;
williamsassignmenthelpfredrick@gmail.com
How To Write A Dissertation Or Thesis

Writing a dissertation or thesis involves a structured process that requires careful planning and execution. Here’s a detailed discussion, covering the key steps in the dissertation writing process.
Step 1: Understand what a dissertation is.

A dissertation is a formal piece of research that follows the standard research process, involving four key steps:
Ask a specific, well-articulated research question(s): Clearly define the focus of your study.
Review existing literature: Explore what other researchers have said about your question.
Undertake your own research: Collect and analyze data in a scientifically rigorous fashion.
Answer your original question(s): Base your conclusions on your analysis findings.
Ensure that your dissertation is a formal piece of research, avoiding personal opinions or preconceived ideas.
Step 2: Find a unique, valuable research topic

Select a research topic that possesses three key attributes:
Clear: Clearly articulate what you plan to research, the questions you want to answer, and the context of your study.
Unique: Address questions that haven’t been answered before, or explore them in a specific context.
Important: Ensure that your research creates value, contributing to the field of research or industry.
Conduct thorough research to identify a topic that is both unique and valuable.
Step 3: Write a convincing research proposal

Craft a research proposal that convinces your university or committee of the worthiness of your research. Your proposal should include:
Clearly articulated, unique, and important topic: Justify why your research is significant.
Review of existing literature: Demonstrate that you’ve done enough reading to identify a clear gap for original research.
Provisional plan: Outline how you will collect and analyze data (methodology).
Show that you’ve done your homework and that your research is worthy of approval.
Step 4: Craft a strong introduction chapter

Use your approved proposal as the basis for your introduction chapter, which should include:
Brief background to the study: Explain the overall area of research.
Problem statement: Identify the problem with the current state of research.
Research questions: Outline the specific questions your study will seek to answer.
Significance of your study: Explain why your research is important and how its findings will be useful.
The introduction sets the scene for your research and justifies your research topic.
Step 5: Undertake an in-depth literature review

Go beyond initial literature review steps and create a comprehensive literature review chapter by:
Reading up: Deep dive into existing literature to understand the current state of research.
Writing up: Synthesize existing research, highlight a research gap, and use the literature to inform your methodology.
The literature review is the foundation on which your research is built.
Step 6: Carry out your own research

Design a research strategy and craft a methodology chapter that explains the “how” of your research:
Design your research strategy: Decide on your research philosophy, methodology, data collection, and analysis strategy.
Execute: Collect and analyze your data based on your research design.
Ensure your research design aligns with your topic, research questions, and data.
Step 7: Present your findings

Present your findings in two chapters — results and discussion. The results chapter should present processed data, while the discussion chapter provides your interpretation of the results:
Results chapter: Present processed data without interpretation.
Discussion chapter: Explain the story the data are telling and interpret the results in relation to your research questions.
Link your discussion back to your research questions outlined in the introduction.
Step 8: Draw a conclusion and discuss the implications

In the conclusion chapter, summarize key findings and discuss their implications:
Key findings: Highlight results directly related to your research questions.
Implications: Explain what your findings mean for industry or research in your area.
Bring your research full circle by answering the “what” and “so what?” questions.
Remember to check your university’s requirements for additional elements like the abstract, reference list, and appendices. Writing a dissertation is a detailed process, but by following these steps, you can craft a high-quality, well-structured document.
Wishing you all the best in writing your Dissertation, we hope this discussion will help.
Incase of any challenges or in need of Guidance during the academic journey;
Email us at;williamsassignmenthelpfredrick@gmail.com
Study Tips For University Students

Introduction
Achieving success as a university student involves mastering effective study methods, time management, and maintaining overall well-being. In this comprehensive discussion, we will major into the top 10 university study tips that can prepare students for the challenges and opportunities that university life presents.
Preview and Review Study Resources
Understanding the importance of previewing study materials before lectures.
Incorporating regular reviews to consolidate knowledge and prepare for new concepts.
Exploring advanced reading techniques for improved comprehension.
2. Customizing Your Note-Taking System
Recognizing the power of note-taking in mastering any subject.
Exploring digital and handwritten note-taking approaches.
Utilizing advanced note-taking apps for organization and efficiency.
Discussing the Cornell Method, mind mapping, and other note-taking strategies.

. Establishing a daily study routine for consistency.
Adapting study habits during holidays to balance academics and festivities.
Creating to-do lists and prioritizing tasks for optimal time management.
Examining time-blocking techniques for enhanced productivity.
4. Setting Goals and Focusing
Setting specific, realistic goals to enhance study sessions.
Avoiding multitasking and using goal-oriented apps for focus.
Exploring the concept of SMART goals in academic settings.

Recognizing the importance of breaks for maintaining attention levels.
Introducing the Pomodoro Technique for efficient study sessions.
Discussing mindfulness and relaxation techniques during breaks.
6. Creating a Suitable Studying Environment
Maximizing productivity by minimizing distractions.
Establishing environmental cues to signal study mode.
Exploring the impact of ergonomics on study efficiency.

Motivating regular study habits by incorporating rewards.
Breaking down tasks into smaller goals for increased control.
Exploring the psychology of rewards and their impact on motivation.
8. Utilizing Study Groups
. Exploring the benefits of studying in groups.
Ensuring structured and accountable study group dynamics.
Discussing effective group communication and collaboration.
9 .Seeking Help When Needed
Overcoming the reluctance to ask for help.
Recognizing the importance of seeking assistance for academic success.
Discussing the role of tutors, mentors, and academic resources.

Understanding the impact of sleep and exercise on academic performance.
Incorporating a consistent sleep schedule and daily exercise routine.
Discussing the link between physical well-being and cognitive function.
Conclusion
In conclusion, success in university requires a holistic approach that encompasses effective study techniques, time management, and self-care. By implementing these ten study tips and delving into related topics, students can not only excel academically but also enhance their overall university experience. Balancing academic commitments with a healthy lifestyle is crucial for long-term success, and these strategies provide a foundation for thriving in the challenging yet rewarding university environment.
We wish you all the best in your University study program.
Incase of any challenges or need assistance and guidance during the process, do not hesitate ,just;
Email us at; williamsassignmenthelpfredrick@gmail.com
10 Research Methods in Psychology

Psychology is a complex field that indulges into the realms of human behavior and mental processes. In the pursuit of understanding these aspects, psychologists employ a myriad of research methods, each tailored to unravel specific dimensions of the human psyche. Whether engaged in experimental investigations or qualitative explorations, these methodologies serve as invaluable tools for therapists, clinicians, and researchers aiming to decipher the complexities of the human mind.
Surveys
Surveys stand as stalwart instruments in the psychologist’s toolkit, facilitating the study of mental health disorders’ prevalence and causative factors. Offering both quantitative and qualitative insights, these inquiries employ random selection techniques to ensure a representative sample. The resultant data not only aids in comprehending human behavior but also serves as a cornerstone for crafting effective treatment strategies.
Tip: Craft well-structured questions and employ random sampling for robust and reliable results.

In the core of qualitative exploration, case studies emerge as profound investigations into the lives of individuals, groups, or communities. By immersing themselves in the core of a subject, psychologists gain miles perspectives on behavior and mental health. Beyond clinical applications, case studies find relevance in diverse fields such as finance, sales, and advertising, offering insights into consumer behavior and decision-making.
Tip: Combine multiple case studies for a comprehensive understanding and ensure triangulation for heightened reliability.
3. Experimental Study
Quantitative in essence, experimental studies play a main role in establishing causal relationships between variables. By manipulating independent variables and observing resultant changes in dependent variables, psychologists gain valuable insights into the external causes of behaviors, both in communities and broader societal contexts.
Tip: Prioritize random assignment for internal validity, strengthening the credibility of causal relationships.
4. Content Analysis:
Involving into the realm of text-based data, content analysis emerges as a powerful method for extracting patterns and themes from patient communication. Whether analyzing interview transcripts or business emails, this technique aids in the development of targeted psychological treatments and proves instrumental in forensic psychology when solving complex behavioral issues.
Tip: Ensure intercoder reliability to enhance the validity of your content analysis.

In the pursuit of synthesizing knowledge, psychologists turn to meta-analysis, a quantitative approach that combines findings from diverse studies. By consolidating information on a specific topic, meta-analysis serves as a comprehensive resource, offering recommendations for future research endeavors and advancing the frontiers of psychology.
Tip: Encompass studies with diverse methodologies for a robust and holistic analysis.
6. Correlational Research
Navigating the unknown landscape of nonexperimental methods, correlational research illuminates relationships between two variables. While not establishing causation, this approach is instrumental in identifying connections, prompting researchers to complement it with causal studies for more nuanced conclusions.
Tip: Clearly communicate the distinction between correlation and causation in research findings.
7. Quasi-Experiment
Akin to traditional experiments but devoid of random participant assignment, quasi-experiments find their niche in studying non-random traits. Particularly valuable when exploring innate qualities, this method enables psychologists to delve into traits that cannot be randomly assigned.
Tip: Transparently acknowledge the limitations associated with quasi-experiments, especially in terms of establishing causal relationships.

Capturing the essence of behavior in its natural habitat, naturalistic observation, a qualitative method, provides a nuanced understanding of how individuals behave in their accustomed settings. Beyond psychology, this method’s applications extend to diverse fields, including technology, sales, and business, offering insights for innovation.
Tip: Integrate naturalistic observation with other methods for a comprehensive grasp of human behavior.
9. Structured Observation
In the controlled environs of a laboratory, structured observation unfolds as a qualitative method to evaluate human behavior systematically. Applied extensively in clinical and medical research, this method aids in understanding how new therapies or medications influence patient behaviors.
Tip: Ensure the relevance of the structured setting to the behavior under scrutiny for heightened external validity.

Harnessing cutting-edge technology, neuroimaging serves as a quantitative method, unveiling the intricacies of the human brain. Techniques like CT scans and MRI enable psychologists to map brain functions, offering profound insights into the interplay between neural processes, thoughts, emotions, and behavior.
Tip: Stay abreast of technological advancements in neuroimaging for continually refined insights into brain activity.
Tips for Conducting Effective Research
Maintain Research Ethics: Uphold ethical standards, ensuring that both research teams and participants are well-versed in procedures, policies, and confidentiality agreements.
Apply the Scientific Method: Consistently adhere to the scientific method, facilitating organized data collection and analysis to enhance result accuracy.
Report Findings: Disseminate research, theories, and analysis within the scientific community. This not only fosters collaboration but also establishes professional authority in the field.
This comprehensive guide encapsulates the diverse array of research methods in psychology, illustrating their applications, nuances, and tips for effective execution. Whether through quantitative experiments or qualitative explorations, psychologists navigate the terrain of human behavior, contributing to the continual evolution of the field.
Wishing you all the best in your Psychology Research and related studies,
For any Challenges or Guidance during the education journey,
Email us at;williamsassignmenthelpfredrick@gmail.com
Nursing Essay

Introduction
Nursing, widely regarded as a challenging academic discipline, demands not only practical skills but also a profound ability to articulate one’s understanding through essays. Despite its predominantly practical nature, nursing essays serve as a critical medium for students to demonstrate their theoretical comprehension of nursing practice. This comprehensive guide aims to provide detailed recommendations, spanning from the methods of choosing a suitable topic to crafting a meticulously structured essay. By adhering to the guidance provided herein, nursing students can significantly enhance their writing skills, expand their knowledge base, and gain invaluable practical experience.
1. The Importance of Nursing

a. Understanding the Role of Nursing Essays
Nursing essays play a major role in assessing a student’s grasp of theoretical aspects of nursing practice. This section delves into the significance of essays in demonstrating clarity of thought, the ability to express arguments, and the implications for academic success.
b. The Link Between Writing Skills and Academic Achievement
Examining how proficient writing contributes to academic success, this subsection explores how essays serve as a direct reflection of a student’s ability to articulate complex ideas and arguments in a coherent manner.
2. Choosing a Suitable Topic

a. The Complexity of Nursing Practice
An in-depth analysis of the broad nature of nursing practice, discussing its various dimensions, functions, and roles. Understanding the complexity of the field is crucial in selecting an engaging and relevant essay topic.
b. Criteria for Choosing a Nursing Essay Topic
This subsection introduces specific criteria for selecting an appropriate essay topic. Emphasizing critical thinking, open-mindedness, and cultural competence, it provides practical advice on avoiding personal biases and ensuring a broad perspective.
c. Examples of Engaging Nursing Essay Topics
Offering a range of potential topics, this section provides concrete examples to inspire nursing students. Topics such as “Cultural Sensitivity in the Context of Advanced Nursing Practice” and “The Role of Informed Consent in Quantitative Research” are explored
3. Evaluating Evidence

a. The Importance of Evidence in Nursing Essays
An exploration of the main role evidence plays in substantiating arguments in nursing essays. This section emphasizes the need for practice-based evidence and the importance of critical evaluation.
b. Distinguishing Types of Evidence
A comprehensive breakdown of different types of evidence, including research-based and experiential evidence. Understanding these distinctions is essential in choosing evidence that aligns with the essay’s objectives.
c. Evaluating the Merits of Evidence
Indulging into the process of evaluating evidence, this subsection discusses the criteria for assessing the authority, reliability, and validity of research designs. Practical tips on making informed judgments about evidence are provided.
Section 4: Understanding Types of Evidence
4. Categorizing Evidence in Nursing Essay

Examining the different types of evidence used in nursing essays and their specific roles. A detailed discussion on how various research designs impact the nature and relevance of evidence.
a. The Significance of Experiential Evidence
Highlighting the importance of experiential evidence in nursing essays, particularly in the analysis of case studies and risk management. Practical insights into incorporating experiential evidence effectively.
b. The Reliability of Research-Based Evidence
Exploring the reliability of evidence derived from research, with an emphasis on the meticulous design of studies to ensure objectivity and validity. A critical discussion on the role of authentic data in supporting claims.
5.The Ultimate Structure of a Nursing Essay

a. Setting the Stage
A comprehensive exploration of the introduction’s role in capturing the reader’s attention, presenting the essay topic, and establishing the rationale for the paper. Practical advice on incorporating hooks, such as questions, statistical data, or quotes, is provided.
b. Crafting a Powerful Thesis Statement
An in-depth examination of the thesis statement, exploring its role as the linchpin of the essay. Examples of strong thesis statements are dissected to illustrate effective positioning and claim formulation.
c. The Main Body: Developing Coherent Arguments
A thorough analysis of the main body’s structure, emphasizing the importance of organizing ideas into clear paragraphs. Practical guidelines on presenting topic sentences, evidence, discussions, and concluding statements are provided.
d. Conclusion: Reinforcing Key Points
A detailed discussion on the conclusion’s role in summarizing key arguments, restating the thesis, and offering recommendations. Practical insights on framing a compelling conclusion that reinforces the essay’s significance.
e. Proofreading and Editing Tips
6. The Importance of Proofreading in Nursing Essays

A critical examination of the proofreading process, highlighting its significance in identifying and rectifying common mistakes. Practical insights into maintaining a scholarly tone and avoiding first-person expression
a. Avoiding Plagiarism Through Proper Citation
An exploration of the importance of proper citation to prevent plagiarism. Guidelines on citing information that is not common knowledge, ensuring academic integrity in nursing essa
b. Evaluating Readability and Coherence
Practical tips on assessing the overall readability and coherence of a nursing essay. Guidance on examining figures, tables, and graphs to enhance visual appeal and effectiveness.
d. Ensuring Consistency in Writing
An exploration of the need for consistency in nursing essays. Practical advice on evaluating the consistency of arguments, statements, and overall presentation
7.Recapitulation of the key points

A concise recapitulation of the key points discussed throughout the guide, reinforcing the critical elements of successful nursing essay writing.
a. Empowering Nursing Students Through Effective Writing
A concluding reflection on how mastering the art of nursing essay writing empowers students to excel academically, contribute meaningfully to the field, and become articulate advocates for healthcare.
Conclusion:
Mastering the art of nursing essay writing is a multifaceted journey that demands a nuanced understanding of the discipline, from choosing a relevant topic to evaluating evidence and crafting a well-structured essay. This comprehensive guide serves as a roadmap for nursing students, providing them with the tools and insights necessary to navigate the complexities of academic writing successfully. By following the detailed recommendations outlined herein, aspiring nurses can not only fulfill the requirements of their coursework but also make substantial contributions to the field through articulate and well-supported essays.
Wishing you all the best in Writing Nursing Essays.
Incase of any Enquiries, Guidance or Challenges faced during the process;
Email us at;
williamsassignmenthelpfredrick@gmail.com
Strategies to Writing a Perfect College Essay

1. Be Authentic
Authenticity is crucial in college essays. It involves selecting a topic or perspective that genuinely reflects who you are. Readers can often discern when a writer is not being authentic, whether it’s through overly embellished language or choosing a topic solely for its perceived impressiveness. Embrace your own voice, use humor naturally, and opt for subjects that hold genuine importance to you, providing a deeper insight into your character.
2. Grab the Reader From the Start
The opening of your essay is a critical opportunity to capture the reader’s attention. A bold statement, a thoughtful quote, an engaging question, or a vivid descriptive scene can set the tone for the entire piece. A clear and compelling thesis statement early on helps guide the reader and establishes the purpose of your essay. This initial impact is essential when competing with numerous other applicants for the admission officer’s attention.
3. Focus on Deeper Themes

Facts and achievements are important, college proffesers are interested in understanding who you are as a person. Delve into deeper themes by connecting your experiences, successes, and adversities to your personal growth. It’s not just about listing accomplishments but demonstrating how those experiences shaped you. This provides a more comprehensive view of your character and journey.
4. Show Don’t Tell

Instead of presenting a mere list of accomplishments, engage the reader by showing scenes and sharing anecdotes. The most captivating essays draw readers into the writer’s world, allowing them to experience the emotional journey. Highlighting the lessons learned and personal insights gained creates a more impactful narrative.
5. Try Doing Something Different
To make your essay stand out, consider approaching your subject from a unique perspective. While common themes like sports-related obstacles or volunteer stories are popular for a reason, exploring a different angle can set you apart. For instance, writing about lessons learned from losses rather than wins can demonstrate resilience and self-awareness.
6. Write With the Reader in Mind

Craft your essay with a clear and logical structure, ensuring that one idea flows naturally into the next. Effective use of transitions between paragraphs enhances the readability of your essay. Anticipate questions the reader might have, and provide the necessary background information. Ensure that the essay is well-organized, avoiding unnecessary wordiness.
7. Write Several Drafts
The importance of multiple drafts cannot be overstated. Setting your essay aside for a few days and returning to it with a fresh perspective often reveals new insights. Starting the writing process early allows sufficient time for revisions. Each draft provides an opportunity to refine your narrative, strengthen arguments, and enhance overall clarity.
8. Read It Aloud

Reading your essay aloud is a valuable editing technique. It helps identify awkward or unnatural-sounding passages. This method allows you to assess the flow of your writing and ensures that your voice remains consistent throughout the essay. It’s an effective way to catch any discrepancies that might be missed during silent reading.
9. Don’t Repeat
Avoid redundancy by not rehashing information already present in other parts of your application. Your essay should contribute new insights, providing a fresh perspective on who you are. Ensure that your essay aligns with the overall theme of your application and directly addresses any questions or prompts given.
10. Ask Others to Read Your Essay

Diverse perspectives are valuable in the editing process. Seek feedback from different individuals, such as teachers, parents, or siblings, to gain varied insights. Pay attention to their interpretations and revise the essay based on their feedback. If any confusion arises among readers, address it through revisions to ensure clarity.
11. Pay Attention to Form
While there might not be strict word limits for college essays, maintaining a balance is crucial. The Common App suggests around 650 words, and adhering to such guidelines is advisable. Additionally, pay attention to formatting details such as readable fonts, proper spacing, and correct dialogue presentation. A visually appealing essay contributes to a positive reader experience.
12. End Your Essay With a “Kicker”

The conclusion is as crucial as the introduction. A “kicker” provides a strong, memorable closing that leaves a lasting impression. It should effectively tie together the key points of your essay, leaving the reader satisfied. Aim for conciseness, coherence, and use vivid details to reinforce the overall message of your essay.
Incorporating these strategies into your college essay writing process can significantly enhance its impact and increase your chances of making a positive impression on admissions officers. Remember, a well-crafted essay can be a powerful tool in differentiating yourself from other applicants
We wish you all the best in your essay writing and studies.
For guidance and and Assistance in all your assignment Help;
Email us at; williamsassignmenthelpfredrick@gmail.com
Viral Infection

Introduction
Viral infections, caused by small germs known as viruses, are prevalent and diverse. They can range from mild conditions such as the common cold to severe and life-threatening illnesses like Ebola or COVID-19. This comprehensive discussion aims to explore various aspects of viral infections, covering their overview, symptoms, causes, diagnosis, management, prevention, outlook, and living with these infections.
Overview
A viral infection occurs when a virus invades the body and utilizes the host’s cells to replicate. Viruses are microscopic pathogens with genetic material (DNA or RNA) encased in a protective protein coat. Unlike bacteria, viruses lack the cellular machinery necessary for self-replication. Instead, they rely on hijacking host cells to reproduce, causing illness in the process.
Understanding Viruses

Viruses, being smaller than bacteria, are visible only under a microscope. They carry genetic information that acts as instructions for replication. In contrast, human cells are complex factories containing the equipment to execute these instructions, such as building proteins and generating more cells. Viruses lack cells and the necessary machinery, making them obligate intracellular parasites.
Distinguishing Viral and Bacterial Infections
Symptoms of viral and bacterial infections often overlap, including fever, cough, and rashes. To differentiate between them, a healthcare provider’s assessment is crucial. Prolonged or worsening symptoms warrant professional evaluation. Various viruses, including herpes and adenoviruses, can cause diverse illnesses, making precise diagnosis crucial for effective treatment.
Types of Viral Infections

Viruses can infect different parts of the body, leading to various types of viral infections. Some common categories include respiratory infections (e.g., common cold, influenza, COVID-19), digestive system infections (e.g., norovirus, hepatitis), viral hemorrhagic fevers (e.g., Ebola, dengue), sexually transmitted infections (e.g., HIV, HPV), exanthemata's infections causing rashes (e.g., chickenpox, measles), neurological infections (e.g., West Nile virus, rabies), and congenital infections transmitted from mother to fetus (e.g., cytomegalovirus, Zika virus).
Risk Factors for Viral Infections
While everyone is susceptible to viral infections, certain factors increase the risk of severe illness. Infants, the elderly, individuals with specific health conditions (diabetes, asthma, COPD), those with weakened immune systems (HIV/AIDS, cancer patients), and pregnant individuals face elevated risks.
Symptoms and Causes
Symptoms of Viral Infections
The symptoms of viral infections vary based on the affected body part but commonly include flu-like symptoms such as fever, body aches, and fatigue. Respiratory infections manifest with sore throat, cough, and sneezing, while digestive system infections cause nausea, vomiting, and diarrhea. Skin conditions like rashes, sores, and warts are also prevalent.
Causes of Viral Infections
Various viruses cause infections in humans, entering the body through the nose, mouth, eyes, anus, genitals, or breaks in the skin. Transmission occurs through direct contact, respiratory droplets, contaminated surfaces, sexual contact, animal bites, or ingestion of contaminated food or water.
Contagious Nature
Almost all viral infections are contagious, relying on human-to-human transmission for survival. The need for living hosts to reproduce drives the contagious nature of viruses.
Diagnosis and Tests

Diagnosing Viral Infections
Healthcare providers can diagnose viral infections by assessing symptoms and conducting examinations. Specific viral identification often involves swabbing the nose or throat or obtaining blood samples. In cases of severe inflammation, imaging techniques like X-rays, ultrasound, MRI, or CT scans may be employed to understand the infection’s impact on internal organs.
Tests for Viral Infections
Laboratory tests on body fluids or tissues, including blood, saliva, sputum, nasal swabs, skin samples, cerebrospinal fluid, urine, stool, and cervical cells (Pap smear), help identify viral DNA/RNA, antibodies, or antigens, aiding in the confirmation of viral infections.
Management and Treatment
Treatment Approaches
While specific antiviral medications are available for some viral infections (e.g., flu, COVID-19, HIV), many viral illnesses, particularly those causing mild symptoms, can be managed at home. Over-the-counter medications, rest, and proper hydration are commonly recommended.
Antiviral Medications
Antiviral medications impede virus replication and are crucial for managing chronic infections or shortening the duration of respiratory illnesses. Specific antivirals exist for influenza, COVID-19, hepatitis B and C, HIV, and certain other viral infections.
Convalescent Plasma and Prophylaxis
In severe cases, convalescent plasma, derived from recovered individuals, is used to introduce antibodies and aid in fighting the infection. Post-exposure prophylaxis, involving antiviral medications and immunoglobulin treatment, can prevent the onset of life-threatening viral infections if administered before symptoms appear.
Limitations of Antibiotics
Antibiotics are ineffective against viral infections and are only prescribed for bacterial infections. Their misuse contributes to antibiotic resistance, emphasizing the importance of accurate diagnosis.
Prevention

Vaccinations
Vaccination is a cornerstone in preventing viral infections. Vaccines are available for numerous viruses, including chickenpox, COVID-19, hepatitis, HPV, influenza, measles, mumps, rubella, polio, rotavirus, rabies, and shingles. Seeking advice from healthcare providers helps determine the appropriate vaccinations based on individual risk factors.
Hygiene Practices
Frequent handwashing, especially during cold and flu seasons, is vital in preventing viral spread. Safe food practices, including proper storage and preparation, contribute to avoiding foodborne viruses. Consistent condom or dental dam use during sexual activity reduces the risk of sexually transmitted infections.
Vector-Borne Viruses
Protecting against vector-borne viruses involves using protective clothing, insect repellents, and mosquito nets. Avoiding contact with wild or aggressive animals and supervising pets outdoors reduces the risk of rabies.
Post-Exposure Prophylaxis
In cases of potential exposure to life-threatening viruses like HIV, rabies, hepatitis B, or chickenpox, immediate post-exposure prophylaxis can prevent illness. Seeking prompt medical attention after exposure is crucial for effective prevention.
Prognosis
Expectations with Viral Infections
The prognosis of viral infections varies, ranging from self-limiting conditions like the common cold to severe and chronic illnesses. Managing less serious infections at home is often possible, while other infections may lead to life-threatening or long-lasting consequences.
Duration of Viral Infections
The duration of viral infections varies widely. Respiratory infections typically last a few days to two weeks, while chronic infections like hepatitis B and C can persist for years. HIV infections are lifelong, requiring ongoing management.
Complications
Viral infections can lead to complications, both immediate and delayed. Severe respiratory illnesses may result in pneumonia, requiring hospitalization. Inflammation in the brain or its lining (encephalitis or meningitis), severe bleeding, reactivation of dormant viruses, and the development of cancer are potential complications associated with viral infections.
Living With Viral Infections

When to Seek Medical Attention
Individuals experiencing viral infection symptoms that persist or worsen after several days should consult a healthcare provider. High-risk individuals with flu or COVID-19 symptoms may benefit from antiviral medications. Immediate medical attention is necessary for those exposed to HIV, rabies, hepatitis B, or chickenpox.
Emergency Situations
Signs of serious infection, such as high fever, difficulty breathing, chest pain, coughing up blood, severe abdominal pain, or mental changes, require immediate medical attention.
Questions for Healthcare Providers
Patients diagnosed with viral infections should inquire about preventing transmission, proper medication usage, expected recovery timelines, symptom management at home, and follow-up appointments.
Conclusion
In conclusion, understanding viral infections is crucial for effective prevention, management, and timely medical intervention. With a focus on vaccination, hygiene practices, and post-exposure prophylaxis, individuals can minimize the risk of contracting and spreading viral infections. While many viral illnesses are self-limiting, recognizing symptoms and seeking appropriate medical care is vital to prevent complications and ensure a healthier outcome. Embracing a proactive approach to viral infection prevention contributes to individual and public health.
For Health Sciences Assignment Help;
Email us at;
williamsliason@outlook.com
Autonomic Nervous System

Introduction
The autonomic nervous system (ANS) constitutes a critical structure of the peripheral nervous system (PNS) responsible for regulating visceral functions. It entirely controls smooth muscles and glands, operating through two primary subdivisions the sympathetic and parasympathetic systems. This comprehensive discussion aims to major into the anatomy, functions, and clinical aspects of the ANS, shedding light on its critical role in maintaining internal organ function and responding to various environmental physiological functions.
1. Sympathetic Autonomic Nervous System

The sympathetic ANS is often associated with the fight or flight response, a mechanism finely tuned to prepare the body for challenging situations. Originating from the thoracolumbar ANS outflow sympathetic pre-ganglionic fibers embark on the processing with distinct routes, influencing organs such as the heart, lungs, and gastrointestinal tract. Notable physiological responses to sympathetic activation include increased cardiac output, arterial vasoconstriction, bronchodilation, and mobilization of glucose stores.
Understanding the sympathetic structure anatomy is crucial for appreciating its diverse connections. The sympathetic pre-ganglionic fibers, predominantly releasing Acetylcholine (Ach) can synapse at different levels within the sympathetic chain or travel to pre-vertebral ganglia. Notably, the adrenal medulla, considered an exception, directly receives pre-ganglionic axons, releasing both adrenaline and noradrenaline into the bloodstream.
2. Parasympathetic Autonomic Nervous System

In contrast, the parasympathetic ANS coordinates the rest and digest response, promoting relaxation and restoration of normal physiological functions after sympathetic arousal. Emerging from the cranial and sacral spinal nerves craniosacral parasympathetic outflow, the parasympathetic pre-ganglionic neurons exert their influence primarily on the upper and lower body, respectively. Key parasympathetic actions reducing heart rate, bronchoconstriction, pupillary constriction, and stimulation of salivation and peristalsis.
A fundamental distinction lies in the neurotransmitters involved in parasympathetic signaling. Both pre- and post-ganglionic neurons release acetylcholine, acting on nicotinic and muscarinic receptors, respectively. This combined action underscores the precise regulation exerted by the parasympathetic system on various target organs.
Receptor Systems and Clinical Correlations

Understanding the receptor systems is important in showing the complexity of autonomic transmission. Nicotinic and muscarinic receptors mediate acetylcholine actions, while adrenergic receptors respond to catecholamines, such as adrenaline and noradrenaline. The varied locations and functions of these receptors elucidate the diverse physiological effects controlled by the ANS.
Clinical correlations, such as the forced expiration, underscore the ANS’s showing involvement in cardiovascular dynamics. This stimulation, involving forced expiration against a closed glottis, provides insights into autonomic function. The work between intrathoracic pressure changes and baroreceptor reflexes showcases the ANS’s role in maintaining cardiovascular homeostasis.
Autonomic Dysfunction and Clinical Implications
Autonomic disorders can significantly impact health, often arising from factors like aging, neuronal damage, or specific medical conditions. Disorders such as diabetic autonomic neuropathy, multiple system atrophy (MSA), and spinal cord disorders underscore the major impact of autonomic dysfunction on various organ systems.
Symptoms of autonomic disorders are diverse, encompassing dizziness, reduced sweating, digestive issues, and urinary abnormalities. Recognizing these symptoms is paramount, prompting individuals to seek medical attention. Diagnostic approaches involve assessing medical history, conducting tests like Tilt table test where light headedness symptoms and electrocardiograms, and evaluating autonomic function through sweat tests and pupillary light reflex tests.
Clinical Relevance

A Valsalva maneuver can be performed by forcing expiration against a closed glottis for ~15 seconds. In clinical settings, this is often achieved by asking patients to try and inflate an empty syringe.
The resulting increase in intrathoracic pressure has a four-phase effect on cardiovascular hemodynamics involving parasympathetic vagal nerve stimulation:
Increased intrathoracic pressure squeezes the pulmonary vessels, increasing venous return to the left heart. This causes a transient increase in stroke volume (SV) increasing cardiac output (CO) and mean arterial pressure (MAP). Baroreceptors in the aortic arch detect this increase in MAP and produce transient bradycardia through the baroreceptor reflex.
2 . Increased intrathoracic pressure prevents venous return to the right heart due to squeezing of the vena cava. This reduces cardiac preload, in turn reducing Stroke volume , Cardiac out , and Mean arterial pressure. The baroreceptor reflect detects this reduced MAP causing an increase in heart rate.
3 .Intrathoracic pressure reduces and normalizes as the Valsalva maneuver is ceased at ~15 seconds. This causes an increase in pulmonary venous coordination due to increased intrathoracic venous capacitance, further decreasing SV, CO, and MAP. This results in a further increase in heart rate through the baroreceptor reflex.
4. As left ventricular preload is restored there is an increase in SV, CO, and MAP. As the heart rate is still elevated there is an overshoot in MAP. This is rapidly corrected by the baroreceptor reflex causing a reflex bradycardia via parasympathetic vagal nerve stimulation. This mechanism returns normal cardiovascular physiology.
The Valsalva maneuver is an effective non-pharmacological first-line treatment for supraventricular tachycardia. The intense parasympathetic vagal stimulation in phase four slows conduction through the AV node and can often terminate supraventricular tachycardias. If this fails, pharmacological methods i.e. IV adenosine are required.
Patients with autonomic dysfunction e.g. diabetic autonomic neuropathy, heart transplant recipients, and patients with high spinal cord injuries lack the normal baroreceptor reflex. As a result, their heart rate will remain constant throughout and their MAP will continue to fall until intrathoracic pressure is released. In this context, Valsalva maneuvers can be used as a diagnostic tool for autonomic neuropathy.
Conclusion
In conclusion, the autonomic nervous system emerges as the main structure of internal organ function, finely balancing the sympathetic and parasympathetic arms. Its anatomy, physiological responses, and clinical implications outweighs its vital role in maintaining physiological homeostasis. As ongoing research continues to reveal the work of autonomic regulation, the significance of this vital system in health and disease becomes increasingly apparent. This exploration serves as a foundational guide, inviting further inquiry into the dynamic understanding of the autonomic nervous system.
For Health Sciences Assignment Help,
Email us at,
williamsfredrick46@gmail.com
14 Reasons to become a Doctor

Introduction
Embarking on a career as a doctor is a monumental commitment, requiring an extensive education, unwavering dedication, and resilience. This detailed exploration aims to involve deep into the 14 compelling reasons to choose the noble profession of a medical doctor. Each reason represents a reality of the face and nature of the medical field, elucidating the diverse experiences, responsibilities, and its rewards associated with this esteemed profession.
1.To Help Others
At the core of a doctor’s vocation lies the fundamental responsibility to save lives and enhance the health of their patients. Exploring through challenging moments in patients’ lives, doctors have a unique opportunity to contribute significantly to their recovery and overall well-being. This shown aspect forms the very heart of the medical profession, acting as a profound motivator for those who choose this career path
2. To Explore Science
The steps involving to become a doctor unfolds as a rigorous educational stages across various scientific disciplines. From foundational studies in physics, chemistry, and biology during undergraduate education to the exploration of specialized subjects like pharmacology, anatomy, pathology, and neurology in medical school, doctors engage with an expansive array of scientific knowledge. This profession not only broadens their understanding but also empowers them to apply scientific principles practically in the life of patient care.
3 .To Have Variety in Your Work
A career in medicine is anonymously dynamic, promising a different experience each day. Doctors find themselves at the forefront of a diverse condition of illnesses and injuries, prompting the utilization of various skills and treatments. This extends beyond the medical cases to include interactions with a wide group of people, including patients, families, and colleagues, making the profession continuously admiring and intellectually engaging.
4. To Collaborate
The medical profession thrives on a team-oriented environment, fostering collaboration with nurses, orderlies, administrators, specialists, and pharmacists. This collaborative ethos not only promotes continuous learning as doctors share insights but also serves as a critical for finding collective solutions to complex medical conditions. Effective teamwork emerges as a cornerstone for successful patient care.
5.To Have Purpose in Your Work
Doctors occupy a crucial role in society, profoundly impacting the lives of individuals and their families. By promoting healthier lifestyles and improving patient health, doctors become stewards in contributing to the well-being of their communities. This sense of purpose adds a profound dimension to the daily work of a doctor.
6. To Educate
With their detailed study, doctors become experts of knowledge, which they can share with patients and colleagues as well. Patient education on health management and lifestyle improvements becomes a crucial aspect of a doctor’s responsibilities. Additionally, some doctors have the unique opportunity to contribute to medical education by mentoring and teaching medical students in teaching hospitals to get the best knowledge.
7. To Have Job Security
The universal demand for medical expertise provides doctors with a reassuring sense of job security. Unlike some professions, doctors rarely face concerns about a lack of competition for their skills. This extensive demand allows for greater flexibility when choosing a work location, catering to a broader spectrum of professional opportunities.
8. To Earn a Good Salary
While salaries in the medical field may vary based on factors such as location, experience, and specialization, doctors generally enjoy competitive remuneration coupled with excellent benefits. Specialized fields, particularly surgery, can qualify for even higher incomes. The financial rewards reflect the substantial investment of time and dedication required in pursuing of a medical career.
9. To Be a Leader
A medical career aligns seamlessly with the aspirations of individuals attached towards leadership roles. Physicians and surgeons often find themselves leading large teams of medical personnel, providing vital and main guidance while taking responsibility for patient outcomes. Exceptional leadership skills may present opportunities for doctors to pursue supervisory roles, further enriching their professional journey.
10. To Learn
Medical professionals encounter many challenges facing new medical conditions and dangers regularly. Liaising with experienced physicians and exposure to diverse cases contribute to a continuous learning environment. This commitment to lifelong learning renders a medical career particularly appealing to those with an insatiable passion for acquiring knowledge.
11. To Test Yourself
The study towards being a doctor is worth undertaking, marked by numerous challenges. Overcoming these challenges becomes a crucial for personal and professional growth. Adapting and continuous self-improvement emerge as integrated face of a physician’s journey, contributing to the development of resilient and resourceful medical professionals.
12. To Solve Problems
Critical thinking stands as a cornerstone of medical practice. Physicians accurately analyze symptoms, review patient conditions, and develop precise diagnosis, considering individual’s symptoms and clinical presentation of a disease condition. The expertise skills required in medicine demand cautiousness , structured thinking, and a balanced approach to well being , proofing the analytical competency of doctors.
13. To Contribute to Breakthroughs
Medicine, like many other scientific fields, is in a delicate state of expanding aided by technological advancements. Staying ahead of recent developments is not just a professional necessity but also an opportunity for doctors to contribute actively to breakthroughs in medical science. Those with an admiration towards medical innovation can explore positions in research hospitals, where their contributions may shape the future of healthcare.
14. To Find New Opportunities
Upon completing the rigorous phases of medical school and residency, doctors find themselves at a point of diverse opportunities. The array of choices includes pursuing specialization in a preferred field, opening a private practice, engaging in community work overseas, majoring into scientific research, contributing to public health initiatives, or transitioning into teaching positions, exploiting the versatility of a medical career.
Conclusion:
A career as a doctor is a field attached with diverse experiences, responsibilities, and opportunities. The 14 reasons explored in this discussion shed light on the main rewards and challenges that accompany the study of a medical profession. From the known satisfaction derived from helping others to the demand for knowledge and the potential to actively contribute to important developments, a medical career beckons those with indriven passion, full dedication, and a commitment to the continuous evolution of their professional journey. The resilience, adaptability, and sense of purpose implanted in the medical profession form the foundation of a vocation that extends far beyond the sense of a mere job, defining a passion that motivates those who aspire to make a meaningful impact on the lives of others through the practice of medicine.
For Health Sciences Assignment Help,
Email us at,
williamsliason@outlook.com
Gastroesophageal reflux disease

Introduction
Gastroesophageal Reflux Disease (GERD) is a chronic condition that affects the gastrointestinal system, leading to the regurgitation of the stomach contents into the esophagus. This discussion aims to explore the aspects of GERD, consisting its causes, symptoms, diagnostic methods, treatment modalities, potential complications, and preventative measures.
I. Causes and Risk Factors
GERD’s pathogenesis primarily generates from the malfunction of the lower esophageal sphincter, a muscular ring separating the esophagus from the stomach. When the lower esophageal sphincter muscle fails to close adequately, stomach contents, including corrosive acids, reflux into the esophagus. Various factors contribute to the development of GERD, ranging from lifestyle choices like alcohol consumption and smoking to physiological factors such as hiatal hernia, obesity, and pregnancy.
II. Symptoms and Manifestations
The symptoms associated with GERD present a spectrum of severity. The main symptom is heartburn, characterized by a burning sensation in the chest. Other prevalent manifestations include the feeling of food stuck behind the breastbone, regurgitation, cough, wheezing, difficulty swallowing, hiccups, hoarseness, and sore throat. Symptom acceleration often occurs during specific activities, such as bending over, lying down, or postprandial periods, with night time symptoms being particularly manifested.
III. Diagnostic Approaches
In cases where symptoms are mild, diagnostic tests may not be immediately necessary. However, persistent or recurrent symptoms may prompt healthcare providers to recommend an upper endoscopy for a detailed examination of the esophagus, stomach, and the initial segment of the small intestine. Additional diagnostic tools include tests measuring the frequency of stomach acid entry into the esophagus, esophageal manometry to assess pressure, and stool occult blood tests to identify potential bleeding.
IV. Treatment Strategies
Managing GERD involves various approaches, beginning with lifestyle modifications. Weight loss, raising up or tilting up the head of the bed, and refraining from lying down post meals constitute fundamental changes. Medications, including antacids, proton pump inhibitors (PPIs), and H2 blockers, are commonly prescribed for symptom relief. In cases resistant to conservative measures, anti-reflux surgery may be considered. Novel endoscopic therapies are emerging as additional options, backing up the evolving landscape of GERD treatment.
V. Prognosis and Potential Complications
While many individuals respond positively to lifestyle changes and medication, a subset may derail the ongoing treatment. Untreated or severe GERD can lead to complications, including exacerbation of asthma, Barrett’s esophagus with an increased risk of cancer, bronchospasm, chronic cough, dental issues, esophageal ulcers, and strictures. Understanding the potential complications emphasizes the importance of proactive management.
VI. When to Seek Medical Attention
Persistent or worsening symptoms despite lifestyle modifications or medication call for prompt medical attention. Warning signs such as bleeding, choking, rapid satiety, frequent vomiting, hoarseness, weight loss, and swallowing difficulties warrant immediate evaluation by healthcare professionals.
VII. Prevention Strategies
Preventing GERD involves a strict approach to lifestyle choices and recognizing potential risks. Maintaining a healthy body weight, adopting dietary modifications, and avoiding specific medications known to exacerbate GERD contribute to prevention. Educating individuals on lifestyle choices and risk factors empowers them to take preventive measures.
Conclusion
Gastroesophageal Reflux Disease is a complex and dynamic condition that demands a broad understanding of its manifestation for effective management. By revealing the various dimensions of GERD, from its underlying causes to treatment modalities and preventative strategies, healthcare professionals and individuals alike can collaboratively explore this challenging condition. A holistic and multidisciplinary approach ensures not only symptom relief but also addresses the long-term implications, promoting a better quality of life for those affected by GERD.
For Health Sciences Assignment Help,
Email us at,
williamsliason@outlook.com
What is mental health?

Mental health is a state of well-being that enables individuals to cope with life stresses, realize their abilities, learn and work effectively, and contribute to their community.
It goes beyond the absence of mental disorders, emphasizing the importance of ongoing wellness and happiness.
Mental health issues affect daily life, relationships, and physical health.
Almost 1 in 5 adults in the U.S. experience mental health problems each year.
Risk Factors for Mental Health Conditions
Socioeconomic factors such as poverty and marginalization increase the risk.
2. Adverse childhood experiences, biological factors, and underlying medical conditions contribute to mental health issues.
3. Chronic stress, depression, and anxiety may result from physical health problems.
Types of Mental Health Disorders
1.Anxiety Disorders:
. Generalized Anxiety Disorder
. Panic Disorder
. Phobias
. Obsessive-Compulsive Disorder
. Post-Traumatic Stress Disorder
2. Mood Disorders:
Major Depression
Bipolar Disorder
Seasonal Affective Disorder
3. Schizophrenia Disorders:
Schizophrenia involves psychotic features, both positive (delusions, hallucinations) and negative (withdrawal, lack of motivation).
Early Signs of Mental Health Disorders
Withdrawal from social activities
Changes in sleep and eating patterns
Persistent feelings of hopelessness
Difficulty completing daily tasks
Thoughts of self-harm or harm to others
Diagnosis
Diagnosing mental health disorders involves a thorough medical history, physical exam, and psychological evaluation.
The American Psychiatric Association’s Diagnostic and Statistical Manual is often used for diagnosis.
Treatment
a. Psychotherapy
Cognitive Behavioral Therapy
Exposure Therapy
Dialectical Behavior Therapy
b. Medication
Antidepressants
Antipsychotics
Anxiolytics
c. Self-help
Lifestyle changes
Relaxation techniques
Support networks
Myths vs. Facts about Mental Health
Intelligence, age, and social status don’t determine mental health.
Teenagers can experience mental health issues.
People with mental health conditions are not necessarily dangerous or violent.
Psychiatric medications are not harmful; they are essential for managing symptoms.
Maintaining Mental Health
Regular exercise, balanced diet, and hydration contribute to mental well-being.
Quality sleep is crucial for mental health.
Relaxing activities, mindfulness, and gratitude practices help manage stress.
Suicide Prevention
Ask direct questions if someone is at immediate risk.
Listen without judgment.
Seek professional help and remove potential harmful objects.
Outlook
Most people can manage mental health symptoms with proper treatment and support.
Recovery may involve learning new coping mechanisms.
Mental health issues are associated with chronic health conditions.
Prevalence of mental disorders peaks in ages 18–25.
Conclusion
Mental health Consists of cognitive, behavioral, and emotional well-being. It involves managing existing conditions while maintaining ongoing wellness. Stress, depression, and anxiety can disrupt mental health, but various treatments, including psychotherapy and medication, are available. Myths about mental health abound, and maintaining mental well-being involves self-care practices and a support network. While mental health disorders are common, proper treatment and support can help individuals lead fulfilling lives.
For Health Sciences Assignment Help,
Email us at;
williamsliason@outlook.com
Osteoporosis in Aging

Introduction
Osteoporosis, a progressive skeletal disorder characterized by reduced bone mass and deteriorating bone quality, poses significant health challenges, especially among the aging population. This discussion involves dynamics of bone health, the factors contributing to osteoporosis, and proactive measures individuals can adopt to protect and strengthen their bones as they age.
1.Understanding Bone Structure and Dynamics
Bones, seemingly solid, have an internal honeycomb-like structure. This structural framework undergoes constant remodeling, with cells building new bone tissue while others dissolve existing bone to release essential minerals. As individuals age, this delicate balance shifts, resulting in a gradual loss of bone density and an increased susceptibility to fractures.
2.Prevalence and Impact of Osteoporosis
Osteoporosis is a widespread concern, affecting over 10 million people nationwide. Its consequences, particularly in Adults, extend beyond fractures, leading to a variety of issues such as disability and loss of dependence. The vulnerability of specific areas, including the;
hips, wrists, and spine, underscores the importance of understanding and addressing this condition.
3.Hormonal Influence and Screening
Estrogen, a crucial hormone, plays a major role in bone formation and regeneration. Postmenopausal women, experiencing a decline in estrogen levels, face a high risk of an increased bone loss. Regular screening, typically recommended for women aged 65 and older, involves non-invasive tests like;
Bone density scan(DXA), measuring bone mineral density. A total score of -2.5 or lower is indicative of osteoporosis.
4.Nutritional Factors
The role of nutrition in maintaining bone health cannot be overstated. Calcium, an essential mineral for bone strength and formation, is obtainable from various dietary sources such as, dairy products and leafy greens. Vitamin D, facilitating calcium absorption, becomes increasingly critical with age. This emphasizes the importance of adequate nutrient intake, either through dietary means or supplements. Specific daily calcium requirements for women over 50 and men over 70 are outlined.
5.Exercise as a Protective Measure
Physical activity, especially weight-bearing exercises like jogging, walking, tennis, and dancing, significantly contributes to bone health. These exercises serve as signals to bone cells, promoting density and reducing the risk of fractures. Conversely, lifestyle choices such as smoking and heavy drinking weaken bones, while certain medications may increase the risk of osteoporosis.
Medical Interventions and Future Prospects
Medical interventions, including medications like bisphosphonates, are commonly prescribed to combat bone loss. Ongoing research is exploring drugs aimed at stimulating bone growth, with parathyroid hormone being a current option. The article discusses the potential of these interventions and highlights the importance of timely medical advice and interventions, even after an osteoporosis diagnosis, to positively impact bone health.
Fall Prevention and Fracture Avoidance
More than 2 million fragility fractures occur annually due to falls, highlighting the need for a comprehensive approach to bone health. Combining efforts to enhance bone strength with fall prevention strategies is crucial. Factors such as balance, environmental hazards, and the type of fall play significant roles in fracture risk. The discussion underscores the effectiveness of exercises that improve balance and coordination, such as slow intentional movement in preventing fractures.
Conclusion
Maintaining optimal bone health is a course that involves a combination of nutrition, exercise, and proactive healthcare measures. Given the critical impact of osteoporosis on aging populations, raising awareness and implementing early intervention strategies are paramount. This comprehensive approach empowers individuals to foresee the risks associated with osteoporosis, ensuring a resilient and active lifestyle in their later years. The discussion concludes by encouraging individuals concerned about their bone health to engage or consult with their healthcare specialists, pressing on the importance of personalized guidance and bone density testing for proactive management.
For Health Sciences Assignment Help;
Email us at;
williamsliason@outlook.com