Health Tips - Blog Posts
🎀🎀
most effective ways to loose weight if you don’t want to st@rve
prioritise sleep (go to bed early and get at least 8 hours)
take any time in your day to walk, get as many steps as you can (preferably 10k+)
eat less meals (ex: skip 1 meal a day, only eat 2)
eat small meals that are healthy/low cal
drink water!! you should drink at least 2L a day! it also helps suppress hunger
sleeping more, eating less, drinking water, and moving your body is going to change your body for the better AND make you feel healthier











What Are My Secrets Of Staying In Shape While Travelling?
I have been a traveller since I was a child. While I would enjoy exploring the different regions, landscapes, cuisines, cultures & languages, I had always paid less attention to a healthy lifestyle.
Well after years of suffering, I finally decided to take control of my health. So, here are my discoveries to staying in shape while travelling.
* Wake Up Early
* Exercise Before You Start Your Journey
* Choose Fun Activities On The Go
* Eat Natural Food
* Hydrate Yourself
* Avoid Junk & Sugary Items
* Take The Stairs Whenever Possible
Health Tips From The Expert 👇
I truly feel blessed to have interviewed Sneha Shah, Head Nutritionist & Lifestyle Expert, Luke Coutinho Holistic Healing Systems.
* According to Sneha, we should first do a research about the cuisine of the region we are visiting so that we can pick up healthier food items focussing on seasonal & local food of the region.
* Also, one should go for small, frequent meals instead of large, heavy meals.
* Eating mindfully takes care of the portion size of each meal.
* Advisable to start with a soup or salad without any dressing.
*Any nauseating problem can be tackled by sipping lemon water or munching on citrus fruits.
* Carrying homemade items like granola bars, mixed nuts or jaggery laddus would make sure that we don't make unhealthy food choices.
*We should carry water in stainless bottles.
*Important to maintain a three hour gap between our last meal & sleep.
Healthy Travelling : A dose of discipline, handful of activities, clean eating habits, a calm mind & peaceful sleep are the key ingredients to a healthy, happy & energetic vacation.
10 Simple Tips for Caring for Your Heart.

The heart, a tireless worker at the core of our well-being, demands our attention and care. As we navigate through Heart Health Month this February, let’s explore ten simple yet impactful tips to ensure our hearts thrive. These practices, ranging from physical activity to laughter and dental hygiene, collectively contribute to a holistic approach to cardiovascular wellness.
1.Cardiovascular Exercise: A Heart’s Best Friend
Engaging in regular cardiovascular or aerobic activities is fundamental for heart health. Following the American Heart Association’s recommendations of 75 minutes of vigorous exercise or 150 minutes of moderate-intensity exercise weekly can significantly boost cardiorespiratory fitness. Activities such as running, cycling, or brisk walking not only elevate heart rate but also enhance overall cardiovascular function. The rhythmic contraction and relaxation of muscles during exercise contribute to improved blood flow and reduced strain on the heart.
2.Embrace a Smoke-Free Lifestyle
Quitting smoking is a paramount step in safeguarding your heart. Smoking damages both the heart and blood vessels, escalating the risk of cardiovascular diseases. Additionally, avoiding second-hand smoke is crucial, as it has been linked to heart attacks and strokes. The harmful chemicals in tobacco smoke lead to the narrowing of blood vessels, increasing the workload on the heart and elevating the risk of high blood pressure.
3.Prioritize Quality Sleep
Adequate sleep, often underestimated, plays a pivotal role in heart health. With at least seven hours of nightly rest, blood pressure lowers, and the body undergoes essential repair processes. Research underscores the correlation between poor sleep and heightened risks of high blood pressure, subsequently increasing the likelihood of heart diseases. Establishing a consistent sleep routine and creating a conducive sleep environment are crucial steps in promoting optimal cardiovascular health.
4.Regular Checkups: A Heart-Healthy Habit
Consistent visits to the doctor for heart health checkups are essential. Assessing risk factors such as diet, blood pressure, cholesterol, and family history enables early detection and management of potential issues. A proactive approach to heart health empowers individuals to make informed lifestyle choices. Regular checkups also provide an opportunity for healthcare professionals to offer personalized guidance on maintaining heart health through tailored interventions.
5.Laughter: The Heart’s Natural Tonic
Laughing, whether through entertainment or social interactions, yields surprising benefits for the heart. The act of laughter reduces artery inflammation, lowers stress hormones, and increases levels of good cholesterol. Integrating humor into daily life becomes a delightful prescription for heart health. Laughter promotes the release of endorphins, the body’s natural feel-good chemicals, which contribute to overall well-being and stress reduction.
6.Dental Hygiene and Heart Connection
Surprising as it may seem, maintaining good dental hygiene contributes to heart health. Studies reveal a link between poor dental health and the presence of bacteria in the bloodstream, impacting heart valves. Simple practices such as regular brushing can significantly decrease the risk of cardiovascular disease. Furthermore, regular dental checkups not only preserve oral health but also serve as a preventive measure against potential cardiovascular complications.
7.Fuel Your Heart with a Healthy Diet
A heart-healthy diet rich in fruits, whole grains, vegetables, and legumes significantly improves blood pressure and cholesterol levels. Steering clear of salty foods and saturated fats is crucial, as they contribute to elevated blood pressure and increased bad cholesterol. Incorporating omega-3 fatty acids, found in fatty fish, flaxseeds, and walnuts, further supports heart health by reducing inflammation and promoting optimal functioning of blood vessels.
8.Maintaining a Healthy Weight: A Heart’s Delight
Striving for and maintaining a healthy weight is a powerful defense against heart disease and high blood pressure. A combination of a balanced diet, regular exercise, and mindful calorie intake promotes overall well-being and cardiovascular health. Excess weight puts additional strain on the heart, leading to conditions such as hypertension and diabetes. Adopting sustainable lifestyle changes, including portion control and regular physical activity, contributes to achieving and sustaining a healthy weight.
9.Hydration: The Heart’s Elixir
Staying adequately hydrated is a simple yet often overlooked aspect of heart care. Considering the heart’s continuous effort in pumping around 2,000 gallons of blood daily, increased water intake supports its optimal functioning. Dehydration can lead to thicker blood, making the heart work harder to pump blood through the vessels. Maintaining proper hydration levels ensures the efficient transport of nutrients and oxygen to cells, promoting overall cardiovascular health.
10.Stay Active, Break Inactivity
Combatting sedentary lifestyles is crucial in preserving heart health. Incorporating simple changes like taking the stairs, walking, playing with pets, or engaging in household chores helps keep the heart active, reducing the risk of cardiovascular diseases. Prolonged sitting has been associated with various health risks, including obesity and heart disease. Regular physical activity not only supports cardiovascular health but also contributes to weight management and overall well-being.
In conclusion, adopting these ten heart-healthy habits provides a comprehensive approach to cardiovascular wellness. Whether it’s the joyous act of laughter, the discipline of regular exercise, or the mindfulness of a balanced diet, each step contributes to the harmonious symphony of a healthy heart. As we celebrate Heart Health Month, let’s embrace these practices and gift our hearts the care they deserve. Through consistent efforts and lifestyle modifications, we can ensure that our hearts continue to beat with vitality and resilience.
Medical students encounter significant academic challenges during their studies, balancing coursework, clinical rotations, research, and personal commitments. Expert Academic Assignment Help offers tailored assistance to meet their needs, providing study materials, tutoring, assignment help, and exam preparation. Beyond academics, it fosters a supportive environment for mentorship and guidance. In essence, Expert Academic Assignment Help is a valuable resource for medical students, empowering them to excel academically and develop into competent healthcare professionals. Contact us at expertassignment46@gmail.com for professional assistance.
ORGANS OF EXCRETION

Excretion, a fundamental process in living organisms, plays a critical role in maintaining internal equilibrium and ensuring the efficient removal of waste products. This detailed discussion will involve deeper into the importance of excretion, the organs involved, their functions, and their contributions to overall health and homeostasis.
Importance of Excretion
Excretion is essential for the survival of all living organisms, from single-celled organisms to complex multicellular organisms like humans. It involves the elimination of metabolic waste products, toxins, and excess substances that accumulate within the body. By removing these waste materials, excretion helps regulate the internal environment, ensuring optimal conditions for cellular function and metabolic processes. Without effective excretory mechanisms, the buildup of waste products would lead to toxicity, impaired physiological function, and ultimately, organismal death.
Organs of Excretion
The human body employs a variety of organs for excretion, each with its own specialized functions and mechanisms for waste elimination. These organs include the skin, liver, large intestine, lungs, and kidneys. While some organs primarily eliminate specific types of waste products, others have multifunctional roles in metabolism, digestion, and detoxification, in addition to excretion.
1. Skin
The skin, the body’s largest organ, serves as a multifunctional barrier between the internal and external environments. In addition to its protective role, the skin participates in excretion through the production of sweat by sweat glands located in the dermis. Sweat, composed of water, salts, and urea, is released through sweat pores onto the skin’s surface, where it evaporates and helps regulate body temperature. Sweating also facilitates the elimination of metabolic wastes, toxins, and excess salts from the body, contributing to overall homeostasis.
2. Liver

The liver, a vital organ located in the upper right abdomen, is involved in numerous metabolic processes, including digestion, detoxification, and the synthesis of essential molecules. As part of its excretory function, the liver processes and eliminates various waste products and toxins from the bloodstream. It metabolizes ammonia, a toxic byproduct of protein metabolism, into urea, a less toxic compound that is excreted by the kidneys in urine. Additionally, the liver excretes bilirubin, a waste product of heme metabolism, into bile, which is then eliminated from the body through the feces.
3. Large Intestine

The large intestine, the final segment of the gastrointestinal tract, plays a crucial role in the absorption of water and electrolytes from undigested food residues. In addition to its role in digestion and water reabsorption, the large intestine serves as a site for the accumulation and elimination of solid waste materials. Bile pigments, such as bilirubin, are excreted into the gastrointestinal tract via bile and eventually eliminated in feces, contributing to the characteristic color of stool.
4. Lungs

The lungs, the primary organs of respiration, also play a role in excretion by removing gaseous waste products, such as carbon dioxide, from the bloodstream. During the process of cellular respiration, carbon dioxide is produced as a byproduct and transported via the bloodstream to the lungs for elimination. Through the process of gas exchange in the alveoli, carbon dioxide is expelled from the body during exhalation, helping to regulate blood pH and maintain acid-base balance.
5. Kidneys

The kidneys are often regarded as the primary organs of excretion in the human body, responsible for filtering waste products and excess substances from the bloodstream and producing urine for elimination. Each kidney contains millions of functional units called nephrons, which play a crucial role in the filtration, reabsorption, and secretion of various substances. Nephrons filter blood to remove waste products, such as urea, creatinine, and uric acid, while reabsorbing essential nutrients and maintaining electrolyte balance. The resulting urine is then transported from the kidneys to the urinary bladder via the ureters and excreted from the body through the urethra during urination.
6. Urinary System

The kidneys, along with the ureters, urinary bladder, and urethra, collectively form the urinary system, which functions to transport, store, and eliminate urine from the body. The ureters carry urine from the kidneys to the urinary bladder, where it is stored until it is expelled from the body through the urethra. The urinary system plays a crucial role in maintaining fluid balance, electrolyte concentration, and pH regulation within the body, thereby supporting overall homeostasis and physiological function.
Conclusion
In conclusion, excretion is a vital process that enables living organisms to eliminate waste products and maintain internal balance. Through the coordinated efforts of various organs, including the skin, liver, large intestine, lungs, and kidneys, the body effectively removes metabolic wastes, toxins, and excess substances, thereby supporting overall health and homeostasis. Understanding the mechanisms of excretion and the roles of excretory organs is essential for appreciating the complexity of physiological regulation and the interconnection of bodily systems. By studying excretory processes, researchers and healthcare professionals can gain insights into disease mechanisms, develop therapeutic interventions, and promote optimal health and well-being.
For students seeking guidance and assistance with their academic assignments, Expert Academic Assignment Help stands out as an invaluable resource. With their unique and top-notch content, they offer solutions to various academic challenges, ranging from essays to research papers ,Clinical case studies and homework. Don’t hesitate to reach out to them for expert assistance and take your academic journey to the next level. For inquiries, contact expertassignment46@gmail.com
Pulmonary Edema

Introduction
Pulmonary edema is a condition that results from the abnormal accumulation of fluid in the lungs, leading to impaired gas exchange and respiratory distress. This comprehensive discourse aims to provide an in-depth analysis of pulmonary edema, covering its pathophysiology, etiology, clinical manifestations, diagnostic modalities, treatment strategies, prevention strategies, and associated complications.
Pathophysiology of Pulmonary Edema

Pulmonary edema develops when there is an imbalance between the hydrostatic and oncotic pressures within the pulmonary vasculature. This imbalance leads to an increase in capillary permeability and the extravasation of fluid into the interstitial space and alveoli of the lungs. Several mechanisms contribute to this process, including increased capillary hydrostatic pressure due to heart failure, increased vascular permeability due to inflammation or injury, and decreased oncotic pressure due to hypoalbuminemia or capillary leak syndrome.
Etiology of Pulmonary Edema
The etiology of pulmonary edema can be categorized into cardiogenic and noncardiogenic causes. Cardiogenic pulmonary edema occurs secondary to heart failure or other cardiac conditions that result in elevated left atrial pressure and pulmonary venous congestion. Noncardiogenic pulmonary edema, on the other hand, is caused by factors unrelated to heart dysfunction, such as acute respiratory distress syndrome (ARDS), aspiration, sepsis, or neurogenic pulmonary edema.
Clinical Manifestations of Pulmonary Edema

The clinical presentation of pulmonary edema varies depending on the underlying cause and severity of the condition. Common symptoms include dyspnea, orthopnea, paroxysmal nocturnal dyspnea, cough, frothy sputum, cyanosis, and crackles on auscultation. Severe cases may progress to respiratory failure, hypoxemia, and hemodynamic instability.
Diagnostic Modalities for Pulmonary Edema

Diagnosing pulmonary edema requires a thorough clinical evaluation, including a detailed medical history, physical examination, and various diagnostic tests. Imaging studies such as chest X-ray, computed tomography (CT) scan, and lung ultrasound can provide valuable information about lung parenchymal changes and the presence of pulmonary congestion. Laboratory tests, including arterial blood gas analysis, brain natriuretic peptide levels, and electrolyte measurements, may also aid in the diagnosis and assessment of disease severity.
Treatment Strategies for Pulmonary Edema
The management of pulmonary edema involves addressing the underlying cause, relieving symptoms, and preventing complications. Initial treatment often includes supplemental oxygen therapy to improve oxygenation and reduce respiratory distress. Diuretics, such as furosemide or bumetanide, are commonly used to reduce fluid overload and alleviate pulmonary congestion. In cases of cardiogenic pulmonary edema, vasodilators, inotropes, or mechanical ventilation may be necessary to improve cardiac function and gas exchange.
Prevention Strategies for Pulmonary Edema
Preventing pulmonary edema requires a broad approach aimed at managing underlying risk factors and promoting healthy lifestyle habits. Patients with known cardiac conditions should adhere to prescribed medications, maintain a low-sodium diet, and monitor fluid intake to prevent fluid retention and exacerbation of heart failure. Individuals at risk of noncardiogenic pulmonary edema should avoid exposure to toxins, practice proper respiratory hygiene, and seek prompt medical attention for respiratory infections or injuries.
Complications of Pulmonary Edema

Untreated or inadequately managed pulmonary edema can lead to several complications, including acute respiratory distress syndrome (ARDS), cardiogenic shock, acute kidney injury, pulmonary hypertension, and death. Prompt recognition and intervention are essential to prevent progression to these life-threatening complications and improve patient outcomes.
Conclusion
Pulmonary edema is a complex and potentially life-threatening condition that requires prompt recognition, accurate diagnosis, and appropriate management. By understanding the underlying pathophysiology, etiology, clinical manifestations, diagnostic modalities, treatment strategies, prevention strategies, and associated complications of pulmonary edema, healthcare providers can optimize patient care and outcomes. Continued research efforts aimed at elucidating the mechanisms underlying pulmonary edema and identifying novel therapeutic targets are essential to further improve patient outcomes and reduce the global burden of this condition.
Embarking on your journey in the field of medicine is both exciting and challenging. As you navigate through your rigorous study period, it’s essential to seek guidance and assistance whenever needed to ensure your success.
At Expert Academic Assignment Help, we understand the demands of medical education and are here to support you every step of the way. Whether you require assistance with assignments, research papers, or exam preparation, our team of experts is dedicated to providing you with the help you need to excel in your studies.
Don’t hesitate to reach out to us for guidance, academic support, or any questions you may have. You can contact us via email at expertassignment46@gmail.com
What Is A Psychotic Disorders?

Introduction
Understanding psychotic disorders requires or encompassing various aspects such as types, symptoms, causes, diagnosis, treatment, prognosis, and preventive measures. Psychotic disorders constitute a diverse array of severe mental illnesses characterized by profound disturbances in cognition, emotion, communication, and behavior, significantly impairing individuals’ ability to function in daily life. Despite the gravity of these conditions, advancements in treatment modalities offer hope for recovery and effective management.
Types of Psychotic Disorders
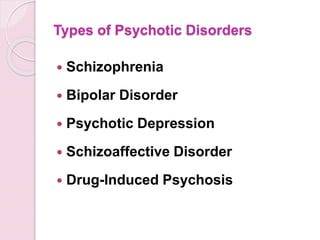
Schizophrenia
This debilitating disorder is characterized by profound alterations in behavior, delusions, and hallucinations persisting for at least six months. It exerts a profound impact on work, relationships, and overall functioning.
Schizoaffective Disorder
Combining features of schizophrenia with mood disorder symptoms like depression or bipolar disorder, schizoaffective disorder presents diagnostic and therapeutic challenges due to its complex symptomatology.
Schizophreniform Disorder
Resembling schizophrenia but with a shorter duration of symptoms (between one to six months), schizophreniform disorder provides insights into the acute phases of psychotic episodes.
Bipolar Psychotic Disorder
Individuals experience sudden, transient episodes of psychotic behavior, often precipitated by extreme stressors, with rapid recovery typically within a month.
Delusional Disorder
Centered around fixed false beliefs (delusions) concerning real-life situations, delusional disorder significantly influences perception and behavior, persisting for at least one month.
Shared Psychotic Disorder
Occurring when one individual’s delusion influences another within a close relationship, shared psychotic disorder elucidates the complexities of interpersonal dynamics in psychosis.
Substance-Induced Psychotic Disorder
Resulting from substance use or withdrawal, this condition underscores the intricate interplay between substance abuse and mental health.
Psychotic Disorder Due to Another Medical Condition
Hallucinations and delusions may arise secondary to underlying medical conditions affecting brain function, necessitating comprehensive evaluation and management.
Paraphrenia
Although not formally recognized in DSM-5, paraphrenia shares similarities with schizophrenia or delusional disorder and typically manifests in late adulthood, potentially associated with neurological factors.
Symptoms of Psychotic Disorders

Hallucinations
Involving perceptual experiences of stimuli that are not present in reality, hallucinations can manifest as auditory, visual, olfactory, gustatory, or tactile phenomena.
Delusions
These fixed, false beliefs persist despite evidence to the contrary, often revolving around themes of persecution, grandiosity, or paranoia.
Disorganized Thinking
Characterized by disjointed or incoherent thought processes, disorganized thinking manifests as impaired logical reasoning, tangential speech, or flight of ideas.
Bizarre Behavior
Individuals with psychotic disorders may exhibit unconventional or socially inappropriate behaviors, including agitation, catatonia, or unusual motor mannerisms.
Social Withdrawal
A hallmark feature of psychotic disorders is the withdrawal from social interactions and activities, often accompanied by a diminished interest in personal hygiene and self-care.
Mood Disturbances
Psychotic disorders may co-occur with mood symptoms such as depression or mania, further complicating the clinical presentation and treatment approach.
Causes of Psychotic Disorders

Genetic Predisposition
While genetic factors contribute to the risk of developing psychotic disorders, the inheritance pattern is complex, involving multiple genes and environmental interactions.
Environmental Factors
Stressful life events, trauma, childhood adversity, and substance abuse play significant roles in precipitating psychotic episodes and exacerbating symptoms.
Neurobiological Abnormalities
Dysregulation of neurotransmitters, particularly dopamine and glutamate, is implicated in the pathophysiology of psychotic disorders, affecting brain regions involved in cognition, perception, and emotion.
Diagnosis of Psychotic Disorders

A comprehensive diagnostic assessment involves obtaining a detailed medical and psychiatric history, conducting a thorough physical examination, performing laboratory tests to rule out medical conditions, and utilizing standardized psychiatric interviews and assessment tools.
Treatment of Psychotic Disorders

Medication
Antipsychotic medications are the cornerstone of pharmacological treatment, targeting symptoms such as delusions, hallucinations, and disorganized thinking. First-generation (typical) and second-generation (atypical) antipsychotics are prescribed based on efficacy and tolerability profiles, with newer agents offering improved side effect profiles and long-acting formulations enhancing treatment adherence.
Psychotherapy
Various forms of psychotherapy, including cognitive-behavioral therapy supportive therapy, and family therapy, complement pharmacotherapy by addressing psychosocial factors, enhancing coping skills, and improving functional outcomes.
Hospitalization
In severe cases or during acute psychotic episodes, hospitalization may be necessary to ensure safety, stabilize symptoms, and initiate intensive treatment interventions.
Prognosis and Recovery
The prognosis of psychotic disorders varies widely among individuals, influenced by factors such as early intervention, treatment adherence, social support, and the presence of comorbid conditions. While some individuals experience rapid symptom improvement and functional recovery, others may require long-term treatment and ongoing support to achieve stability and prevent relapse.
Prevention of Psychotic Disorders

Although prevention of psychotic disorders remains challenging, early intervention, identification of high-risk individuals, and mitigation of modifiable risk factors such as substance abuse and stress can reduce the incidence and severity of psychotic episodes. Public education, de stigmatization efforts, and access to mental health services promote awareness and facilitate timely intervention.
In conclusion, psychotic disorders represent complex and mental illnesses that profoundly impact individuals’ lives and necessitate comprehensive evaluation and treatment. By addressing the diverse array of symptoms, underlying neurobiological abnormalities, and psychosocial factors, clinicians can optimize treatment outcomes and support individuals in achieving improved quality of life and functioning. Through ongoing research, education, and advocacy, the understanding and management of psychotic disorders continue to evolve, offering hope for enhanced outcomes and reduced burden on affected individuals and society as a whole.
Students immersed in the fields of medical and psychology, seeking guidance from Expert Academic Assignment Help can be transformative. Whether it’s for assignments, studies, or navigating the challenges of medical School, expert assistance can provide clarity, direction, and invaluable insights. By reaching out to expertassignment46@gmail.com students can access personalized support, comprehensive resources, and expert advice to excel in their academic pursuits and lay a solid foundation for their future careers. Don’t hesitate to seek guidance — your academic success and professional growth are worth investing in.
Cirrhosis Of The Liver

Introduction
Cirrhosis stands as a challenge in the narrative of liver disease, marking the culmination of a complex interplay of factors that converge to undermine the organ’s structural integrity and functional capacity. This condition, characterized by the progressive accumulation of scar tissue within the liver parenchyma, holds a cascade of physiological network that reverberate throughout the body, manifesting in a spectrum of symptoms and complications. From its inner onset to its profound implications for morbidity and mortality, cirrhosis generate the intricate interplay between genetic predisposition, environmental influences, and individual behaviors.
In this comprehensive discussion, we embark on an exploration of the multifaceted dimensions of cirrhosis, traversing its etiological underpinnings, clinical manifestations, diagnostic modalities, therapeutic strategies, and avenues for prevention and self-care. By delving into the intricacies of cirrhosis, we endeavor to elucidate the imperative of early recognition, proactive intervention, and holistic management in ameliorating its adverse sequelae and fostering optimal outcomes for affected individuals
Pathophysiology of Cirrhosis

Central to the pathogenesis of cirrhosis lies a complex interplay of molecular and cellular events that precipitate the gradual transformation of healthy hepatic tissue into fibrotic scar tissue. At the heart of this process lies fibrogenesis, wherein a multitude of cellular players, including hepatic stellate cells, inflammatory mediators, and extracellular matrix proteins, triggers a profibrotic milieu in response to persistent liver injury and inflammation. The ensuing deposition of collagen-rich scar tissue disrupts the structure of the liver lobules, impeding normal hepatocellular function and vascular dynamics.
Symptoms and Clinical Manifestations

The clinical presentation of cirrhosis spans a broad spectrum, reflecting the diverse array of physiological derangements engendered by advanced liver disease. Early-stage cirrhosis may manifest subtly, with nonspecific symptoms such as fatigue, malaise, and vague abdominal discomfort, often eluding timely diagnosis. However, as the disease progresses, overt signs of hepatic decompensation emerge, including jaundice, ascites, hepatic encephalopathy, and gastrointestinal bleeding, heralding the onset of life-threatening complications. Moreover, cirrhosis exerts systemic effects beyond the confines of the liver, precipitating coagulopathy, renal dysfunction, and metabolic disturbances.
Etiology and Risk Factors
Cirrhosis arises from an influence of etiological insults, encompassing a diverse spectrum of predisposing factors that contribute to hepatocellular injury and fibrogenesis. Foremost among these is chronic alcohol abuse, which inflicts direct hepatotoxic effects and potentiates oxidative stress and inflammatory cascades within the liver microenvironment. Additionally, viral hepatitis infections, particularly hepatitis B and C, constitute major drivers of cirrhosis worldwide, underscoring the imperative of vaccination and antiviral therapy in disease prevention and management. Other contributing factors include nonalcoholic fatty liver disease, autoimmune disorders, hereditary hemochromatosis, and biliary tract diseases, each exerting a unique influence on cirrhosis pathogenesis.
Diagnostic Modalities

Accurate diagnosis forms the linchpin of effective cirrhosis management, necessitating a judicious amalgamation of clinical symptoms, laboratory investigations, imaging modalities, and histopathological evaluation. Liver function tests serve as indispensable tools for gauging the synthetic and metabolic capacity of the liver, while imaging studies such as ultrasound, computed tomography (CT), and magnetic resonance imaging (MRI) afford insights into hepatic morphology, vascular dynamics, and the presence of focal lesions. Despite their utility, these modalities may be supplemented by liver biopsy, which remains the gold standard for assessing the degree of fibrosis and guiding therapeutic decisions, albeit fraught with procedural risks and sampling variability.
Treatment Strategies

While cirrhosis represents a chronic and irreversible condition, therapeutic interventions are geared toward monitoring disease progression, alleviating symptoms, and forestalling the onset of complications. Pharmacological therapies, including hepatoprotective agents, antifibrotic agents, and symptom-based medications, aim to attenuate hepatic inflammation, inhibit fibrogenesis, and ameliorate symptom burden in cirrhotic patients. Furthermore, endoscopic interventions such as variceal band ligation and trans jugular intrahepatic portosystemic shunting play a major role in the management of portal hypertension and its sequelae, including variceal bleeding and refractory ascites. For select individuals with end-stage liver disease, liver transplantation offers a definitive therapeutic option, affording a second lease on life and circumventing the inexorable progression of cirrhosis-related complications.
Self-Care and Lifestyle

Empowering individuals with cirrhosis to adopt proactive self-care measures constitutes a cornerstone of comprehensive disease management, emphasizing the role of lifestyle modifications, dietary interventions, and preventive strategies in optimizing health outcomes. Lifestyle modifications, including abstinence from alcohol, adherence to a liver-friendly diet, regular exercise, and smoking cessation, are paramount in attenuating hepatic inflammation, promoting metabolic homeostasis, and mitigating cardiovascular risk factors in cirrhotic patients. Additionally, vaccination against hepatitis viruses, avoidance of hepatotoxic medications, and judicious monitoring of comorbid conditions serve as essential pillars of preventive care, safeguarding against disease exacerbations and fostering long-term wellness in individuals with cirrhosis.
Conclusion
Cirrhosis emerges as a complex and a dangerous disease, syndrome characterized by progressive hepatic fibrosis, compromised organ function, and a plethora of systemic manifestations. The etiological heterogeneity of cirrhosis underscores the need for a personalized and multidisciplinary approach to disease management, Focusing to the unique pathophysiological mechanisms and clinical manifestations inherent to each individual. Through timely diagnosis, targeted interventions, and collaborative care, healthcare providers can mitigate the burden of cirrhosis, optimize patient quality of life, and prolong survival in affected individuals. As we navigate complexities of cirrhosis, a concerted emphasis on preventive measures, patient education, and therapeutic innovations holds the key to unlocking a brighter prognosis for those afflicted by this formidable liver disease.
Medical students encounter significant academic challenges during their studies, balancing coursework, clinical rotations, research, and personal commitments. Expert Academic Assignment Help offers tailored assistance to meet their needs, providing study materials, tutoring, assignment help, and exam preparation. Beyond academics, it fosters a supportive environment for mentorship and guidance. In essence, Expert Academic Assignment Help is a valuable resource for medical students, empowering them to excel academically and develop into competent healthcare professionals. Contact at expertassignment46@gmail.com for assistance guidance.
Diabetes

Introduction to Diabetes
Diabetes, a metabolic disorder characterized by chronic hyperglycemia, arises from abnormalities in insulin secretion, insulin action, or both. The condition’s prevalence has reached epidemic proportions globally, with significant health, economic, and social implications.
Types of Diabetes

Type 1 Diabetes: This autoimmune disease results from the destruction of pancreatic beta cells, leading to absolute insulin deficiency. Genetics and environmental triggers play pivotal roles in its pathogenesis. Despite being less common than Type 2 diabetes, its onset during childhood or adolescence significantly impacts individuals’ lives.
Type 2 Diabetes: Predominantly a disorder of insulin resistance, Type 2 diabetes accounts for the majority of diabetes cases worldwide. Lifestyle factors, genetic predisposition, and obesity contribute to its development. Its insidious onset often leads to delayed diagnosis and increased risk of complications.
Gestational Diabetes: Occurring during pregnancy, gestational diabetes poses risks to both maternal and fetal health. Hormonal changes and insulin resistance characterize its pathophysiology. Effective screening and management are crucial to prevent adverse outcomes.
Other Types of Diabetes: Variants like MODY, LADA, and secondary diabetes present unique challenges in diagnosis and management, requiring tailored approaches to care.
Epidemiology and Prevalence
Diabetes prevalence varies across demographics, with disparities observed in age, gender, ethnicity, and socioeconomic status. The escalating burden of diabetes underscores the urgent need for targeted prevention and management strategies.
Symptoms and Causes

Hyperglycemia-induced symptoms like polyuria, polydipsia, and unexplained weight loss serve as clinical indicators for diabetes diagnosis. Understanding the complex interplay of genetic, environmental, and lifestyle factors elucidates the condition’s etiology.
Complications
Diabetes complications encompass a spectrum of microvascular and macrovascular disorders, significantly impacting quality of life and life expectancy. From diabetic retinopathy to cardiovascular disease, nephropathy, neuropathy, and diabetic foot complications, the ripple effects of uncontrolled diabetes are profound.
Diagnosis and Tests

Accurate diagnosis relies on comprehensive evaluation, including fasting glucose, oral glucose tolerance tests, and hemoglobin A1c measurements. Screening recommendations aim to identify at-risk individuals early, facilitating timely intervention and risk reduction.
Management and Treatment
Diabetes management strategies encompass pharmacotherapy, lifestyle modifications, patient education, and multidisciplinary care. Individualized treatment plans address glycemic control, blood pressure management, lipid optimization, and prevention of complications.
Prevention
Prevention initiatives target modifiable risk factors through health promotion, public health interventions, and community engagement. Emphasizing the role of nutrition, physical activity, and behavioral changes empowers individuals to mitigate their diabetes risk.
Outlook and Prognosis
Prognostic factors such as glycemic control, adherence to therapy, comorbidity burden, and psychosocial support influence long-term outcomes. Enhanced collaboration among healthcare providers, policymakers, and stakeholders is essential to improve diabetes prognosis globally.
Living With Diabetes

Coping with diabetes requires resilience, self-management skills, and social support networks. Empowering individuals through education, self-monitoring tools, and peer support enhances their capacity to navigate the challenges of daily diabetes management.
Impact on Individuals and Society
Diabetes exerts a profound socioeconomic burden, encompassing healthcare costs, productivity losses, and reduced quality of life. Addressing the psychosocial dimensions of diabetes care is integral to fostering holistic well-being and societal resilience.
Future Directions and Research

Advancements in diabetes research, including precision medicine, digital health technologies, and novel therapeutics, offer promising avenues for disease management and prevention. Collaborative research endeavors aim to translate scientific discoveries into tangible clinical benefits.
Conclusion
In conclusion, diabetes represents public health challenge necessitating a comprehensive, patient-centered approach. By fostering awareness, promoting early detection, and advancing evidence-based interventions, we can mitigate the impact of diabetes on individuals, families, and communities worldwide.
Medical students encounter significant academic challenges during their studies, balancing coursework, clinical rotations, research, and personal commitments. Expert Academic Assignment Help offers tailored assistance to meet their needs, providing study materials, tutoring, assignment help, and exam preparation. Beyond academics, it fosters a supportive environment for mentorship and guidance. In essence, Expert Academic Assignment Help is a valuable resource for medical students, empowering them to excel academically and develop into competent healthcare professionals. Contact at expertassignment46@gmail.com for assistance.
10 Common Dental Problems

Introduction
Maintaining optimal dental health is crucial not only for a winning smile but also for overall well-being. However, numerous individuals encounter common dental issues that can affect their quality of life. From tooth decay to gum disease, understanding these problems and their treatments is essential for preventing complications and preserving oral health. This comprehensive guide explores ten prevalent dental problems and outlines effective treatment options for each, empowering individuals to make informed decisions about their dental care.
1.Tooth Decay

Tooth decay, also known as dental caries, is a pervasive dental issue caused by the accumulation of plaque and the subsequent erosion of tooth enamel. This section delves into the causes, symptoms, and treatment options for tooth decay, emphasizing the importance of preventive measures such as regular brushing, flossing, and dental check-ups.
2. Gum Disease

Gingivitis and periodontitis are two stages of gum disease characterized by inflammation and bacterial infection of the gums. Exploring the risk factors, symptoms, and management strategies for gum disease sheds light on the importance of proper oral hygiene practices and professional dental interventions in preserving gum health.
3.Bad Breath

Halitosis, or bad breath, can stem from various underlying factors such as poor oral hygiene, dry mouth, and underlying medical conditions. This segment examines the causes of bad breath and highlights the significance of comprehensive dental assessments and tailored treatment plans to address this common concern effectively.
4.Sensitive Teeth

Tooth sensitivity, characterized by discomfort in response to hot, cold, or sweet stimuli, often results from enamel erosion or underlying dental issues. Delving into the potential causes and management options for sensitive teeth underscores the role of personalized dental care in alleviating discomfort and enhancing oral comfort.
5.Cracked or Broken Teeth

Cracks or fractures in teeth can result from trauma, bruxism (teeth grinding), or other factors, leading to pain and functional impairment. This section explores the diagnostic procedures and treatment modalities available for repairing cracked or broken teeth, emphasizing the importance of prompt intervention to prevent further damage.
6.Receding Gums

Receding gums, characterized by the exposure of tooth roots due to gum tissue loss, can result from various factors, including poor oral hygiene and genetic predispositions. Analyzing the causes, consequences, and treatment approaches for receding gums underscores the significance of preventive measures and professional interventions in preserving gum health.
7. Root Infection

Root infections, often resulting from untreated cavities or trauma, can lead to severe pain and dental abscesses if left untreated. This segment elucidates the diagnostic techniques and treatment options for root infections, highlighting the role of root canal therapy in alleviating symptoms and preserving tooth structure.
8. Enamel Erosion

Enamel erosion, characterized by the gradual loss of tooth enamel due to acidic and sugary dietary habits, poses significant challenges to dental health. Exploring preventive strategies and restorative treatments for enamel erosion underscores the importance of dietary modifications and proactive dental care in preserving tooth structure and function.
9. Dry Mouth

Xerostomia, or dry mouth, can result from various factors, including medication side effects and underlying medical conditions. This section examines the causes, symptoms, and management strategies for dry mouth, emphasizing the importance of hydration and lifestyle modifications in alleviating discomfort and preventing oral complications.
10. Teeth Grinding
Bruxism, characterized by involuntary teeth grinding or clenching, can lead to tooth wear, jaw pain, and headaches. Exploring the underlying causes and treatment options for bruxism underscores the importance of stress management and protective dental appliances in mitigating symptoms and preserving dental health.
Conclusion
In conclusion, understanding and addressing common dental problems are essential steps toward maintaining optimal oral health and overall well-being. By recognizing the signs and symptoms of tooth decay, gum disease, and other dental issues, individuals can seek timely intervention and preventive care to mitigate risks and preserve their smiles. Through a combination of proper oral hygiene practices, regular dental check-ups, and personalized treatment plans, individuals can navigate common dental challenges with confidence and achieve lasting oral health. Embracing proactive dental care and seeking professional assistance when needed are crucial components of a comprehensive approach to dental wellness.
In exploring and pursuing your dental studies, we wish you all the best in becoming a dentist. In case you encounter challenges or need guidance during this study period, do not hesitate to contact us.
Email at;williamsassignmenthelpfredrick@gmail.com
The pathophysiology of hypertension

Introduction
Hypertension, or high blood pressure, is a complex medical condition affecting a significant proportion of the global population. Despite its prevalence, there remains uncertainty regarding its pathophysiology, with essential hypertension constituting a substantial portion where no single identifiable cause is found. This comprehensive discussion aims to delve into the physiological mechanisms involved in the development of hypertension, exploring factors such as cardiac output, peripheral resistance, the renin-angiotensin-aldosterone system, the autonomic nervous system, endothelial dysfunction, genetic factors, and intrauterine influences.
Cardiac Output and Peripheral Resistance

Maintaining normal blood pressure relies on the delicate balance between cardiac output and peripheral vascular resistance. Essential hypertension often involves a normal cardiac output but elevated peripheral resistance, primarily determined by small arterioles. The role of smooth muscle cells, calcium concentration, and structural changes in arteriolar vessel walls contribute to the irreversible rise in peripheral resistance.
Renin-Angiotensin System

The renin-angiotensin system plays a crucial role in blood pressure regulation. Renin, released in response to various stimuli, initiates the conversion of angiotensinogen to angiotensin I, which is then converted to the vasoconstrictor angiotensin II. This system also stimulates aldosterone release, promoting sodium and water retention. While the circulating system may not be directly responsible for essential hypertension, local renin-angiotensin systems in organs like the kidney, heart, and arterial tree gain significance in regulating regional blood flow.
Autonomic Nervous System

Sympathetic nervous system stimulation affects arteriolar constriction and dilation, playing a pivotal role in maintaining normal blood pressure. Although the exact role of epinephrine and norepinephrine in hypertension etiology remains unclear, drugs blocking the sympathetic nervous system demonstrate therapeutic efficacy.
Endothelial Dysfunction

Vascular endothelial cells, producing vasoactive agents like nitric oxide and endothelin, play a key role in cardiovascular regulation. Endothelial dysfunction, implicated in essential hypertension, involves impaired production of nitric oxide. This dysfunction, once established, becomes irreversible, highlighting its primary nature in hypertension.
Vasoactive Substances

Various vasoactive substances, such as bradykinin, endothelin, atrial natriuretic peptide, and ouabain, influence sodium transport and vascular tone. These substances contribute to the delicate balance in maintaining normal blood pressure.
Genetic Factors
Genetic predisposition significantly contributes to hypertension, with specific mutations linked to disorders like Liddle’s syndrome, glucocorticoid-remediable aldosteronism, and others. The intricate interplay of multiple genes makes it challenging to pinpoint individual contributions.
Intrauterine Influences
Fetal influences, particularly birth weight, emerge as determinants of adult blood pressure. The Barker hypothesis suggests a link between low birth weight, metabolic abnormalities, and hypertension in later life. However, the role of genetic factors in this relationship requires further exploration.
Diastolic Dysfunction

Hypertensive left ventricular hypertrophy leads to impaired diastolic relaxation, affecting ventricular input during exercise. This dysfunction contributes to increased atrial pressure, pulmonary congestion, atrial fibrillation, and potential complications like pulmonary edema.
Conclusion
In conclusion, understanding the pathophysiology of hypertension involves a multifaceted exploration of various physiological mechanisms. While essential hypertension remains a complex and often multifactorial condition, advancements in research shed light on factors such as cardiac output, peripheral resistance, the renin-angiotensin system, the autonomic nervous system, endothelial dysfunction, genetic influences, and intrauterine factors. A comprehensive understanding of these elements is crucial for developing effective therapeutic strategies and preventive measures against the global burden of hypertension.
We hope this helps in improving our comprehension of the Hypertension condition. All the best in your journey in the medical field.
Incase of any challenges' and in need of professional guidance, contact;
Expert Academic Assignment Help at;
williamsassignmenthelpfredrick@gmail.com
Osteoporosis in Aging

Introduction
Osteoporosis, a progressive skeletal disorder characterized by reduced bone mass and deteriorating bone quality, poses significant health challenges, especially among the aging population. This discussion involves dynamics of bone health, the factors contributing to osteoporosis, and proactive measures individuals can adopt to protect and strengthen their bones as they age.
1.Understanding Bone Structure and Dynamics
Bones, seemingly solid, have an internal honeycomb-like structure. This structural framework undergoes constant remodeling, with cells building new bone tissue while others dissolve existing bone to release essential minerals. As individuals age, this delicate balance shifts, resulting in a gradual loss of bone density and an increased susceptibility to fractures.
2.Prevalence and Impact of Osteoporosis
Osteoporosis is a widespread concern, affecting over 10 million people nationwide. Its consequences, particularly in Adults, extend beyond fractures, leading to a variety of issues such as disability and loss of dependence. The vulnerability of specific areas, including the;
hips, wrists, and spine, underscores the importance of understanding and addressing this condition.
3.Hormonal Influence and Screening
Estrogen, a crucial hormone, plays a major role in bone formation and regeneration. Postmenopausal women, experiencing a decline in estrogen levels, face a high risk of an increased bone loss. Regular screening, typically recommended for women aged 65 and older, involves non-invasive tests like;
Bone density scan(DXA), measuring bone mineral density. A total score of -2.5 or lower is indicative of osteoporosis.
4.Nutritional Factors
The role of nutrition in maintaining bone health cannot be overstated. Calcium, an essential mineral for bone strength and formation, is obtainable from various dietary sources such as, dairy products and leafy greens. Vitamin D, facilitating calcium absorption, becomes increasingly critical with age. This emphasizes the importance of adequate nutrient intake, either through dietary means or supplements. Specific daily calcium requirements for women over 50 and men over 70 are outlined.
5.Exercise as a Protective Measure
Physical activity, especially weight-bearing exercises like jogging, walking, tennis, and dancing, significantly contributes to bone health. These exercises serve as signals to bone cells, promoting density and reducing the risk of fractures. Conversely, lifestyle choices such as smoking and heavy drinking weaken bones, while certain medications may increase the risk of osteoporosis.
Medical Interventions and Future Prospects
Medical interventions, including medications like bisphosphonates, are commonly prescribed to combat bone loss. Ongoing research is exploring drugs aimed at stimulating bone growth, with parathyroid hormone being a current option. The article discusses the potential of these interventions and highlights the importance of timely medical advice and interventions, even after an osteoporosis diagnosis, to positively impact bone health.
Fall Prevention and Fracture Avoidance
More than 2 million fragility fractures occur annually due to falls, highlighting the need for a comprehensive approach to bone health. Combining efforts to enhance bone strength with fall prevention strategies is crucial. Factors such as balance, environmental hazards, and the type of fall play significant roles in fracture risk. The discussion underscores the effectiveness of exercises that improve balance and coordination, such as slow intentional movement in preventing fractures.
Conclusion
Maintaining optimal bone health is a course that involves a combination of nutrition, exercise, and proactive healthcare measures. Given the critical impact of osteoporosis on aging populations, raising awareness and implementing early intervention strategies are paramount. This comprehensive approach empowers individuals to foresee the risks associated with osteoporosis, ensuring a resilient and active lifestyle in their later years. The discussion concludes by encouraging individuals concerned about their bone health to engage or consult with their healthcare specialists, pressing on the importance of personalized guidance and bone density testing for proactive management.
For Health Sciences Assignment Help;
Email us at;
williamsliason@outlook.com
Interesting Nursing Research Topics To Choose

Childhood Nursing
Antibiotics Impact on Childhood Immunities
Antibiotics have revolutionized modern medicine, significantly improving the prognosis for many infectious diseases. However, the impact of antibiotics on childhood immunities is a multifaceted topic that warrants careful examination. While antibiotics target harmful bacteria, they may also affect the delicate balance of the immune system in developing children.
Research could delve into the long-term consequences of antibiotic use during childhood, exploring how it may influence the development of the immune system. Are there specific types of antibiotics that pose greater risks? What role do probiotics play in mitigating the potential negative effects of antibiotics on the immune system? Understanding these dynamics is crucial for optimizing pediatric care and ensuring the long-term health of children.
Effects of Childhood Exposure to Environmental Pollutants
Children are particularly vulnerable to environmental pollutants, and exposure during early life stages can have lasting health implications. Research in this area could focus on specific pollutants, such as air pollutants, heavy metals, or endocrine disruptors, and their impact on children’s health.
Exploring the effects of second-hand smoke inhalation during early life stages is particularly relevant. What are the respiratory and cardiovascular consequences of childhood exposure to second-hand smoke? How does environmental pollution contribute to respiratory conditions in children, and what preventive measures can be implemented?
Ethics of Pediatric Care
The ethical dimensions of pediatric care are intricate, involving considerations of autonomy, beneficence, and justice. Topics within this realm could include ethical dilemmas faced by pediatric nurses, such as decision-making in cases where parental and child interests may conflict.
Research may also explore the ethical implications of emerging technologies in pediatric care. For instance, what are the ethical considerations surrounding genetic testing in children? How can nurses navigate the ethical challenges posed by advances in pediatric treatments and interventions?
Genetic Factors of Diabetes in Children
The increasing prevalence of diabetes in children raises questions about the genetic factors contributing to this trend. Research in this area could delve into the genetic markers associated with pediatric diabetes, exploring the hereditary aspects of the disease.
Understanding the interplay between genetic predisposition and environmental factors is crucial. What role do lifestyle factors play in the manifestation of diabetes in genetically predisposed children? How can nurses incorporate genetic counseling into pediatric diabetes management to empower families with the knowledge needed for preventive strategies?
How Health in Children Can Affect Their Health Later in Life
The concept that early life experiences can shape health outcomes in adulthood is a key area of interest. Research could investigate the link between childhood health and long-term health trajectories. Are there specific childhood health indicators that serve as predictors of adult health issues?
Exploring the mechanisms through which childhood health influences adulthood health can guide nursing interventions. How can nurses promote healthy behaviors in children that have lasting effects on their well-being? What preventive measures can be implemented during childhood to mitigate the risk of chronic diseases in adulthood?
Adult Nursing
Analyzing the Benefits of Collaborative Nursing
Collaborative nursing involves interdisciplinary teamwork to enhance patient care outcomes. Research in this area could explore the benefits of collaborative nursing practices in diverse healthcare settings. What are the positive outcomes associated with collaborative care, such as improved patient satisfaction, reduced hospital readmissions, or enhanced treatment adherence?
Understanding the factors that contribute to successful collaboration is essential. How do effective communication and shared decision-making impact collaborative nursing efforts? What challenges do nurses face in interprofessional collaboration, and how can these challenges be addressed to optimize patient care?
Analyzing the Causes of Depression
Depression is a prevalent mental health concern affecting a significant portion of the adult population. Research into the causes of depression can provide valuable insights into preventive measures and targeted interventions. This could involve exploring the interplay between genetic, environmental, and psychological factors in the development of depression.
Investigating the role of adverse childhood experiences in predisposing individuals to depression in adulthood is a pertinent avenue. How can nurses identify individuals at risk based on early life experiences? What interventions can be implemented to break the cycle of depression rooted in childhood trauma?
Ethics of Data Collection in Adult Health Care
The ethical considerations surrounding data collection in adult health care are paramount, especially in the era of electronic health records and data-driven healthcare. Research could delve into the ethical challenges nurses face in collecting, storing, and utilizing patient data.
Exploring the perspectives of patients regarding data privacy and consent is crucial. How do patients perceive the use of their health data for research purposes? What safeguards can be implemented to ensure ethical data practices in adult health care settings?
Evolution of Nursing in a Specific Time Period
The evolution of nursing over time reflects changes in healthcare practices, societal attitudes, and technological advancements. Research in this area could focus on a specific time period, examining how nursing roles, responsibilities, and education have transformed.
For example, a study could explore the evolution of nursing during a period of significant healthcare reform. What were the key drivers of change, and how did nurses adapt to new models of care? Understanding historical contexts can inform current nursing practices and guide future developments in the profession.
Nonchemical Treatments for Bipolar Disorders
Bipolar disorders present unique challenges in terms of management and treatment. Research into nonchemical treatments for bipolar disorders can provide valuable alternatives or complementary approaches to medication-based interventions.
Exploring the efficacy of psychotherapy, cognitive-behavioral interventions, and lifestyle modifications in managing bipolar disorders is essential. How can nurses incorporate nonchemical treatments into holistic care plans for individuals with bipolar disorders? What role does patient education play in promoting self-management strategies for bipolar conditions?
Midwifery Nursing
Analysis of Caseload and Quality of Care for Underrepresented Groups
Midwives play a crucial role in maternal and infant care, yet disparities in care outcomes persist among underrepresented groups. Research in this area could investigate the caseloads and quality of care provided to women from marginalized communities.
Examining the experiences of midwives in catering to diverse caseloads can provide insights into challenges and opportunities. How do midwives adapt their care approaches to address the unique needs of underrepresented populations? What strategies can be implemented to ensure equitable access to high-quality midwifery care?
Analysis of Childbirth Experiences of Women with Autism
Pregnancy and childbirth can pose unique challenges for women with autism spectrum disorders. Research could explore the childbirth experiences of women with autism, considering factors such as sensory sensitivities, communication preferences, and support needs.
Understanding the specific needs of this population can inform midwifery practices and improve the overall childbirth experience. What adjustments can be made in maternity care settings to accommodate the needs of women with autism? How can midwives collaborate with other healthcare professionals to provide holistic care for pregnant individuals with autism?
Nonchemical Pain Management in Labor
Labor pain is a central aspect of childbirth, and nonchemical pain management approaches are gaining attention. Research in this area could focus on the effectiveness of non-pharmacological pain management methods during labor.
Exploring techniques such as hydrotherapy, massage, acupuncture, and mindfulness can provide valuable insights. How do these nonchemical methods influence pain perception and labor outcomes? What role can midwives play in promoting and facilitating the use of non-pharmacological pain management strategies during childbirth?
Role of Midwifery in Emergency Care
While childbirth is often a natural process, emergencies can arise, requiring swift and effective interventions. Research could investigate the role of midwives in emergency care.
Conclusion
In this expansive discussion, we have explored a variety of nursing research topics across different specializations. Each topic presents unique challenges, opportunities, and areas for further exploration within the field of nursing. Whether focusing on pediatric care, mental health, women’s health, or health care management, the diverse range of topics reflects the major areas to consider.
For further assistance and guidance, link to us on williamsliason@outlook.com
Medical attention
About medical attention and being the first to believe to yourself.
Some of us form into ppl pleasers due to certain circumstances. Sometimes it is even hard to tell what do you feel if nobody believes you you feel this way. Than, if unfortunately you become ill, if nobody believes you... You might accidentally believe them instead of yourself. But our body is wise, and it gives emotional and physical signals to our brain with a reason! No one is living this life from your first day to your last day, in your shoes, in your skin - except YOU. You have the widest perspective on your life story. Only you live and feel the consequences of believing them and abandoning yourself. And it is not your fault, it is all you have known till that moment. Please forgive yourself, because... At any moment you have the choice to be the first human being on earth to believe you, to be by your side. I don't know if it would help, but I am alread believing you. Everything you have gone through, any emotion and sensation you have - it all makes perfect sense to me, it is important, it deserves to be seen and respected. So if you don't get the right medical attention, please don't stop searching for better options. Even if you need to pause for such long period of time to regain trust, to save money if possible... The moment you can, please keep moving forward, because YOU deserve to find those kind compassionate allies in life - who will care, who will listen, who will help without making you smaller than the equal human being you are. Because your essence is awsome and you deserve to get the help you need ❤️